Antibiotic stewardship programs: What are their impact on resistance?
Assess the effectiveness of antibiotic stewardship programs in reducing resistance rates and promoting responsible antibiotic use in clinical settings.
Antibiotic Resistance: A Tug-of-War between Drugs and Microbes
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-30
Antibiotics have long been hailed as one of the greatest medical breakthroughs of the 20th century, offering a powerful weapon against infectious diseases that once claimed millions of lives. However, the overuse and misuse of these wonder drugs have led to the rise of antibiotic resistance, a global health crisis that threatens to undo the progress made in modern medicine.
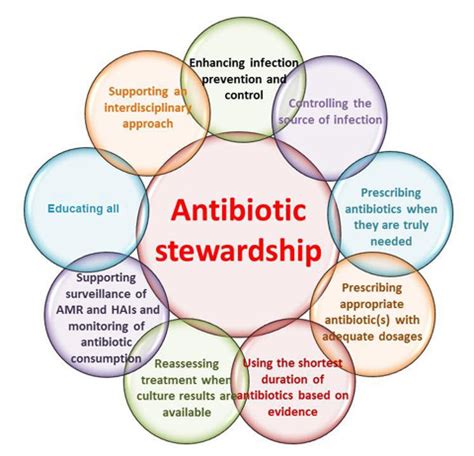
As bacteria evolve to outsmart the very drugs designed to eliminate them, healthcare providers and policymakers have turned to antibiotic stewardship programs as a potential solution. These coordinated efforts aim to promote the responsible use of antibiotics, minimizing the emergence and spread of resistant microbes. But just how effective are these programs in the ongoing battle against antibiotic resistance?
The Vicious Cycle of Resistance
Antibiotic resistance occurs when bacteria develop the ability to withstand the effects of a particular drug, rendering it ineffective. This can happen when antibiotics are overused or used inappropriately, allowing resistant strains to thrive and proliferate. As resistance spreads, the pool of effective antibiotics dwindles, making it increasingly challenging to treat even common infections.
This vicious cycle has far-reaching consequences. Infections caused by resistant bacteria can be more severe, require longer hospital stays, and result in higher healthcare costs. In some cases, they may even prove fatal, as no effective treatment options remain.
The Rise of Antibiotic Stewardship
Recognizing the gravity of the situation, healthcare organizations and regulatory bodies have implemented antibiotic stewardship programs to address the problem. These initiatives aim to optimize the use of antibiotics, ensuring they are prescribed and administered correctly, while also promoting alternative treatments and preventive measures.
- Surveillance and Monitoring: Tracking antibiotic use and resistance patterns to identify problem areas and guide interventions.
- Education and Training: Providing healthcare professionals with the knowledge and skills to prescribe antibiotics judiciously.
- Antimicrobial Stewardship Teams: Multidisciplinary teams that review and optimize antibiotic prescribing practices.
- Antibiotic Restrictions: Implementing policies to limit the use of certain antibiotics, particularly those considered "last-resort" options.
- Infection Prevention and Control: Implementing measures to reduce the spread of infections, such as hand hygiene and environmental cleaning.
The Impact of Antibiotic Stewardship
While the implementation of antibiotic stewardship programs is still relatively recent, the available evidence suggests that they can have a significant impact on reducing antibiotic resistance rates and promoting responsible antibiotic use.
Studies have shown that these programs can lead to a decrease in the incidence of resistant infections, such as methicillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile. They have also been associated with a reduction in the use of broad-spectrum antibiotics, which are more likely to contribute to the development of resistance.
Moreover, antibiotic stewardship programs have been linked to improved patient outcomes, including shorter hospital stays, lower mortality rates, and reduced healthcare costs. By ensuring that antibiotics are used judiciously, these programs help preserve the effectiveness of existing antimicrobial agents and potentially delay the emergence of new resistant strains.
The Road Ahead
While the implementation of antibiotic stewardship programs is a step in the right direction, the fight against antibiotic resistance is far from over. Continued efforts are needed to educate healthcare providers, engage with the public, and develop new antimicrobial therapies to overcome this global health challenge.
As we navigate this complex issue, one thing is clear: the success of antibiotic stewardship programs will be crucial in determining the future of modern medicine. By striking the right balance between the appropriate use of antibiotics and the preservation of their effectiveness, we can hope to turn the tide in the ongoing battle against resistant microbes.
What are your thoughts on the role of antibiotic stewardship programs in addressing the problem of antibiotic resistance? Share your insights and experiences in the comments below.
User comments
More Topics to Explore
How do bacteria develop antibiotic resistance?
Explore the various mechanisms through which bacteria develop resistance to antibiotics and the implications for healthcare practices.
Can antibiotic resistance be reversed?
Discuss the potential methods to reverse antibiotic resistance and the feasibility of such approaches in clinical settings.
What are the latest advancements in combating antibiotic resistance?
Share insights on the cutting-edge strategies and technologies being developed to tackle antibiotic resistance effectively.
Antibiotic resistance in animals: How does it affect human health?
Examine the link between antibiotic use in animals and the development of resistance that can impact human health.
How can personalized medicine help in addressing antibiotic resistance?
Explore the role of personalized medicine in tailoring antibiotic treatments to individual patients for improved effectiveness and reduced resistance.
How do biofilms contribute to antibiotic resistance?
Investigate the role of biofilms in protecting bacteria from antibiotics and enhancing resistance mechanisms, posing challenges in treatment.
The role of genetic mutations in antibiotic resistance: Are there new insights?
Discuss recent findings on genetic mutations that contribute to antibiotic resistance and their implications for developing targeted therapies.
Antibiotic cycling: Does it mitigate resistance or exacerbate it?
Debate the effectiveness of antibiotic cycling strategies in controlling resistance patterns versus the risks of promoting further resistance development.
How can multidisciplinary collaboration combat antibiotic resistance effectively?
Explore the importance of interdisciplinary teamwork among healthcare professionals, researchers, and policymakers in addressing antibiotic resistance on a global scale.