Integrating Antivirals and Antibiotics: Navigating the Complexities of Infection Management
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Apr-09
As the global healthcare landscape continues to evolve, the need for effective and comprehensive infection management strategies has become increasingly crucial. One promising approach that has garnered significant attention in recent years is the integration of antivirals and antibiotics to tackle various types of infections. However, this integration is not without its challenges, and healthcare professionals must navigate a delicate balance to ensure the most favorable outcomes for patients.
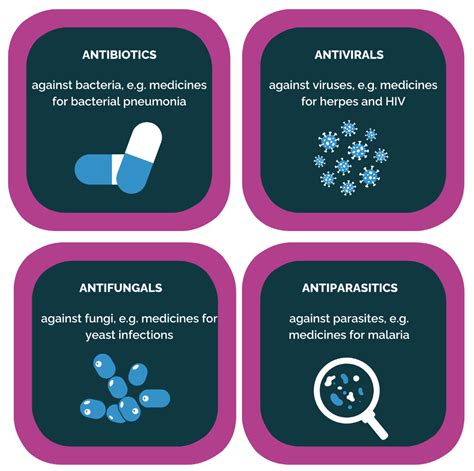
At the heart of this discussion lies the fundamental differences between antivirals and antibiotics. Antivirals are designed to target and disrupt the replication of viruses, while antibiotics are primarily focused on eradicating bacterial infections. The complex interplay between these two classes of drugs, coupled with the diverse nature of infectious agents, presents healthcare providers with a multifaceted challenge.
One of the primary hurdles in integrating antivirals and antibiotics is the potential for drug interactions. The simultaneous administration of these medications can lead to unexpected pharmacokinetic and pharmacodynamic interactions, which can either diminish the effectiveness of the drugs or result in adverse side effects. Careful monitoring and management of these interactions are essential to ensure the safety and efficacy of the treatment regimen.
Another significant challenge lies in the antimicrobial resistance crisis. As pathogens continue to evolve and develop resistance to various antimicrobial agents, the effectiveness of both antivirals and antibiotics can be compromised. This dynamic landscape requires healthcare professionals to stay abreast of the latest research and guidelines, regularly reassessing treatment strategies to ensure they remain effective against emerging resistant strains.
Despite these challenges, the integration of antivirals and antibiotics also presents numerous opportunities for improved infection management. By leveraging the complementary mechanisms of action of these two drug classes, clinicians can potentially enhance the overall therapeutic efficacy and spectrum of coverage. This approach may be particularly beneficial in cases of co-infections, where both viral and bacterial agents are present, or in situations where the underlying etiology is unclear.
Moreover, the integration of antivirals and antibiotics can contribute to antimicrobial stewardship efforts. By judiciously combining these medications, healthcare providers can minimize the overuse and inappropriate prescription of antibiotics, which is a key driver of antimicrobial resistance. This, in turn, can lead to better patient outcomes and reduced healthcare costs associated with the management of resistant infections.
As the field of infection management continues to evolve, the integration of antivirals and antibiotics holds significant promise. However, navigating the complexities of this approach requires a deep understanding of pharmacology, microbiology, and clinical decision-making. Healthcare professionals must collaborate closely with multidisciplinary teams, stay informed of the latest research, and continuously refine their strategies to overcome the challenges and capitalize on the opportunities presented by this innovative approach.
What do you see as the most critical considerations in integrating antivirals and antibiotics for effective infection management? Share your insights and experiences in the comments below.