Challenges in Engaging Healthcare Providers in Antibiotic Stewardship
Address the obstacles faced in involving healthcare providers in antibiotic stewardship initiatives. Exchange strategies for increasing participation and commitment from clinicians and staff.
Engaging Healthcare Providers in Antibiotic Stewardship: Overcoming the Challenges
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-21
The judicious use of antibiotics is a critical aspect of healthcare, yet encouraging consistent participation in antibiotic stewardship programs remains an ongoing challenge for many healthcare facilities. Antibiotic stewardship aims to optimize the selection, dosage, and duration of antibiotic therapy, ultimately reducing the spread of antibiotic-resistant bacteria. However, despite the recognized importance of these initiatives, getting healthcare providers to actively engage in stewardship efforts can be an uphill battle.
One of the primary obstacles lies in the inherent complexity of antibiotic prescribing. Clinicians often face significant time constraints, competing priorities, and a deluge of information when deciding on the appropriate antibiotic regimen. Balancing patient outcomes, concerns about antimicrobial resistance, and institutional guidelines can be a daunting task, particularly in the fast-paced environment of acute care settings. Providers may feel that antibiotic stewardship programs add an extra layer of bureaucracy, interfering with their clinical decision-making autonomy.
Furthermore, a lack of comprehensive educational resources and training on antibiotic stewardship principles can contribute to provider hesitancy. Many clinicians may not have received formal instruction on the nuances of antibiotic selection, dosing, and de-escalation strategies during their medical education. This knowledge gap can lead to a perception that stewardship initiatives are overly burdensome or unnecessary.
Organizational culture and institutional priorities can also play a significant role in provider engagement. If antibiotic stewardship is not clearly articulated as a top organizational priority, supported by strong leadership, and integrated into the overall quality improvement framework, healthcare providers may be less inclined to prioritize these initiatives. Providers may feel that their efforts will not be recognized or rewarded, further diminishing their motivation to participate.
To overcome these challenges and foster greater engagement, healthcare organizations must adopt a multifaceted approach. One key strategy is to provide comprehensive, tailored educational opportunities for clinicians, nurses, and other healthcare staff. This can include interactive workshops, online modules, and case-based discussions that highlight the clinical and public health benefits of antibiotic stewardship. By equipping providers with the necessary knowledge and tools, organizations can empower them to make more informed decisions and feel confident in their stewardship efforts.
Equally important is the establishment of clear, evidence-based guidelines and protocols that integrate seamlessly into the provider's workflow. By aligning stewardship recommendations with existing clinical pathways and decision-support systems, organizations can minimize the perceived burden on healthcare providers, making it easier for them to incorporate stewardship principles into their daily practice.
Moreover, a collaborative, multidisciplinary approach to antibiotic stewardship can foster a sense of shared responsibility and collective ownership among healthcare providers. Engaging clinicians, pharmacists, infection preventionists, and other key stakeholders in the development and implementation of stewardship initiatives can help overcome silos and promote a culture of accountability.
Ultimately, the success of antibiotic stewardship programs hinges on the active engagement and commitment of healthcare providers. By addressing the unique challenges faced by clinicians, healthcare organizations can create an environment that encourages and supports their participation in these crucial initiatives. As we continue to confront the growing threat of antimicrobial resistance, fostering provider engagement in antibiotic stewardship will be essential in safeguarding the future of effective, high-quality patient care.
What strategies has your organization implemented to increase healthcare provider participation in antibiotic stewardship? Share your experiences and insights in the comments below.
User comments
More Topics to Explore
How to Implement an Effective Antibiotic Stewardship Program?
Discuss strategies and tips for successfully implementing an antibiotic stewardship program in healthcare settings. Share insights on overcoming challenges and ensuring sustainability.
The Role of Technology in Antibiotic Stewardship Programs
Explore the impact of technology on antibiotic stewardship efforts. Share examples of how digital tools and healthcare technology can enhance antibiotic prescribing practices and improve patient outcomes.
Measuring Success: Key Metrics for Evaluating Antibiotic Stewardship Programs
Delve into the essential metrics and indicators used to assess the effectiveness of antibiotic stewardship programs. Share insights on measuring outcomes, tracking progress, and demonstrating the impact of stewardship efforts.
The Patient Perspective: Involving Patients in Antibiotic Stewardship
Explore the importance of patient involvement in antibiotic stewardship initiatives. Discuss ways to educate and engage patients in promoting responsible antibiotic use and combating antibiotic resistance.
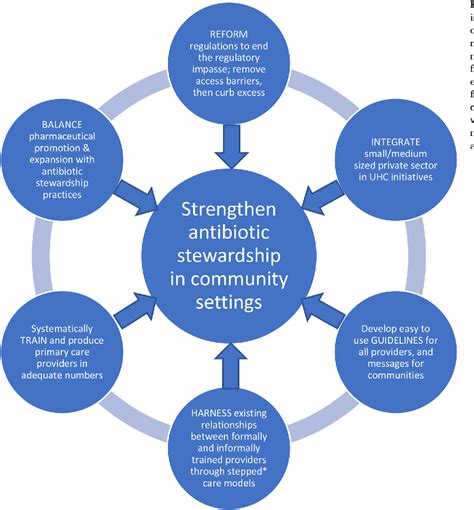
Antibiotic Stewardship in Community Settings: Best Practices and Challenges
Share best practices and address challenges related to implementing antibiotic stewardship programs in community healthcare settings. Exchange insights on tailoring stewardship strategies to suit the unique needs of community-based care.
Innovations in Antibiotic Stewardship: Novel Approaches and Technologies
Explore cutting-edge innovations and novel technologies shaping antibiotic stewardship practices. Discuss emerging trends and disruptive solutions that are revolutionizing the landscape of antibiotic stewardship programs.
Antibiotic Stewardship Training: Empowering Healthcare Professionals
Discuss the importance of training healthcare professionals in antibiotic stewardship principles and practices. Share resources, experiences, and strategies for equipping clinicians with the knowledge and skills to be effective stewards of antibiotics.
Collaborative Approaches to Antibiotic Stewardship: Building Partnerships for Impact
Explore the benefits of collaborative initiatives in strengthening antibiotic stewardship programs. Share examples of successful partnerships between healthcare organizations, policymakers, and other stakeholders to drive impactful stewardship efforts.
Antibiotic Stewardship Communication Strategies: Engaging Stakeholders Effectively
Exchange insights on effective communication strategies for engaging stakeholders in antibiotic stewardship programs. Discuss the importance of clear and targeted messaging to drive awareness, promote adherence, and foster a culture of responsible antibiotic use.