The growing threat of antiviral resistance has become a major concern in the field of infectious disease management. As viruses continue to evolve and develop mechanisms to evade the effects of individual antiviral drugs, healthcare providers are increasingly turning to combination therapy as a means of enhancing treatment efficacy and overcoming this challenge.
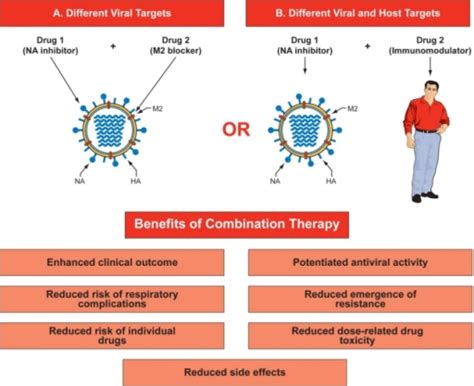
Combination therapy, the simultaneous use of two or more antiviral agents, has emerged as a promising strategy to combat the emergence of antiviral resistance. The rationale behind this approach is rooted in the concept of targeting multiple viral pathways or mechanisms simultaneously, making it more difficult for the virus to develop resistance to the entire treatment regimen.
When a virus is exposed to a single antiviral drug, it can often rapidly develop mutations that confer resistance to that specific agent. However, when multiple drugs with different mechanisms of action are used in combination, the virus would need to acquire multiple, simultaneous mutations to overcome the entire treatment approach. This significantly reduces the likelihood of the virus developing resistance, as the probability of such complex, coordinated mutations occurring is much lower.
Moreover, combination therapy can also provide other benefits, such as enhanced antiviral efficacy, broader spectrum of activity, and the potential for lower dosages of individual drugs, thereby reducing the risk of side effects. By leveraging the synergistic effects of multiple antiviral agents, combination therapy can potentially lead to faster viral suppression, improved clinical outcomes, and a higher barrier to the development of resistance.
The application of combination therapy has been particularly successful in the management of human immunodeficiency virus (HIV) infection, where the use of highly active antiretroviral therapy (HAART) has dramatically improved treatment outcomes and reduced the emergence of resistant strains. This approach has served as a model for the use of combination therapy in other viral diseases, such as hepatitis C virus (HCV) and influenza.
In the case of HCV, the introduction of direct-acting antiviral (DAA) combination regimens has revolutionized the treatment landscape, leading to significantly higher rates of sustained virological response (SVR) and a reduced risk of resistance development. Similarly, the use of combination influenza treatments, including the co-administration of neuraminidase inhibitors and other antiviral agents, has shown promise in enhancing treatment efficacy and mitigating the impact of drug resistance.
As researchers and clinicians continue to explore the potential of combination therapy, it is crucial to understand the underlying mechanisms, the selection of appropriate drug combinations, and the optimization of dosing strategies. Ongoing studies and clinical trials are exploring various combination approaches, evaluating their safety, tolerability, and long-term efficacy in combating antiviral resistance.
In conclusion, the strategic use of combination therapy has emerged as a crucial approach in the fight against the growing threat of antiviral resistance. By leveraging the synergistic effects of multiple antiviral agents, healthcare providers can enhance treatment outcomes, improve patient care, and contribute to the ongoing efforts to combat the evolving challenges posed by viral infections. As the field of antiviral therapeutics continues to progress, the development and implementation of effective combination therapy strategies will remain at the forefront of strategies to combat drug resistance and improve patient outcomes.
What are your thoughts on the role of combination therapy in overcoming antiviral resistance? Share your insights and experiences in the comments below.
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-21