How can effective infection control practices reduce the risk of sepsis?
Discuss the link between infection control measures and sepsis prevention outcomes.
Maintaining Proper Infection Control to Prevent Sepsis
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-30
Healthcare-associated infections (HAIs) are a serious concern, leading to significant patient morbidity and mortality. One of the most life-threatening complications of HAIs is sepsis - a severe and often deadly immune response to infection. However, by implementing effective infection control practices, healthcare facilities can significantly reduce the risk of sepsis and other devastating outcomes.
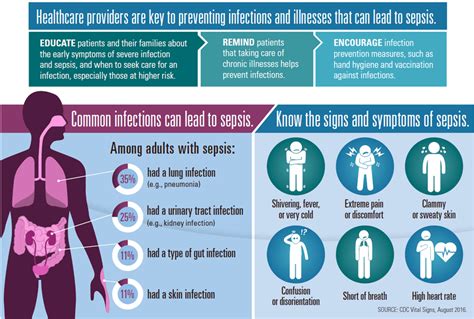
Sepsis arises when the body's immune system goes into overdrive while trying to fight an infection, triggering a cascade of physiological changes that can rapidly lead to organ dysfunction, shock, and even death. Patients with weakened immune systems, such as the elderly, those with chronic illnesses, or those who have undergone invasive medical procedures, are at an especially high risk of developing sepsis.
Proper infection control is crucial in preventing the spread of infectious pathogens that can cause sepsis. This includes thorough hand hygiene, the use of personal protective equipment (PPE) like gloves and gowns, and the disinfection of medical equipment and high-touch surfaces. Effective sterilization of surgical instruments and proper wound care techniques are also essential to minimize the risk of post-operative infections.
Furthermore, antimicrobial stewardship programs in healthcare settings can help curb the development of antibiotic-resistant bacteria, which are a major contributor to the rise of deadly infections like sepsis. By promoting the judicious use of antibiotics and monitoring for emerging resistance patterns, these programs can preserve the effectiveness of our limited antimicrobial arsenal.
Early recognition and prompt treatment of infections are also key to preventing sepsis. Healthcare providers must be vigilant in identifying the signs and symptoms of sepsis, such as fever, rapid heart rate, and altered mental status, and initiate appropriate interventions without delay. Rapid administration of antibiotics and fluid resuscitation can be life-saving measures for patients with sepsis.
In addition to these clinical interventions, patient education plays a vital role in sepsis prevention. Empowering patients and their families to recognize the early warning signs of sepsis and to advocate for prompt medical attention can significantly improve outcomes. Healthcare facilities should also prioritize patient safety by fostering a culture of transparency and continuous quality improvement.
By implementing a comprehensive infection control program that encompasses hand hygiene, PPE use, disinfection, antimicrobial stewardship, and early sepsis recognition, healthcare organizations can significantly reduce the risk of sepsis and other deadly infections. Investing in these critical measures can not only save lives but also reduce the significant financial burden associated with HAIs and their complications.
As we continue to grapple with the challenges of healthcare-associated infections, it is clear that effective infection control practices hold the key to preventing the devastating consequences of sepsis. By prioritizing these measures, we can ensure a safer, healthier future for patients and healthcare providers alike.
User comments
More Topics to Explore
How can we effectively prevent sepsis in healthcare settings?
Discuss best practices and protocols for preventing sepsis within healthcare facilities.
What are the key measures to prevent sepsis in vulnerable populations?
Explore targeted prevention strategies for at-risk groups to reduce sepsis incidence.
How can early recognition of sepsis improve prevention efforts?
Share insights on the importance of early sepsis detection in preventing its progression.
What role do antibiotics play in the prevention of sepsis?
Examine the use of antibiotics as a preventive measure for sepsis and their impact.
Are there specific vaccination strategies to prevent sepsis?
Delve into the role of vaccines in sepsis prevention and any specific vaccination strategies.
What are the nutritional interventions that can aid in preventing sepsis?
Explore the impact of nutrition on sepsis prevention and specific dietary interventions.
How can proper wound care contribute to sepsis prevention?
Share insights on the importance of wound care in preventing sepsis and promoting healing.
What are the benefits of early fluid resuscitation in sepsis prevention?
Discuss the advantages of timely fluid resuscitation in preventing sepsis-related complications.