How Do Cephalosporins Compare to Fluoroquinolones as Antibiotics?
Join this discussion to compare and contrast cephalosporins and fluoroquinolones in terms of their spectrum of activity, common uses, and potential side effects, fostering an exchange of knowledge among members.
Cephalosporins vs. Fluoroquinolones: Comparing Antibacterial Powerhouses
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-27
As the medical community continues to navigate the complex landscape of antimicrobial resistance, the debate around the relative strengths and weaknesses of different antibiotic classes remains a topic of keen interest. Two such classes that have garnered substantial attention are the cephalosporins and the fluoroquinolones.
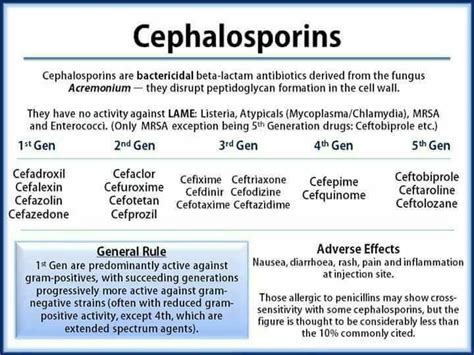
Cephalosporins are a family of beta-lactam antibiotics derived from the fungus Acremonium, with a structure similar to penicillins. They are renowned for their broad-spectrum activity, effectively targeting a wide range of both Gram-positive and Gram-negative bacteria. This versatility has made cephalosporins a mainstay in the treatment of numerous bacterial infections, including pneumonia, meningitis, urinary tract infections, and skin and soft tissue infections.
On the other hand, fluoroquinolones are a class of synthetic antibiotics that target the bacterial enzymes DNA gyrase and topoisomerase IV, which are essential for DNA replication and cell division. This unique mechanism of action allows fluoroquinolones to exhibit potent activity against a diverse array of both Gram-positive and Gram-negative pathogens, including those resistant to other antibiotic classes.
When it comes to their comparative spectrum of activity, both cephalosporins and fluoroquinolones demonstrate impressive coverage. Cephalosporins are particularly effective against Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria gonorrhoeae, while fluoroquinolones excel at targeting Pseudomonas aeruginosa, Escherichia coli, and Klebsiella pneumoniae. However, it is important to note that the specific activity of each subclass within these broader categories can vary, and clinicians must carefully consider the individual agent and the local resistance patterns when selecting the appropriate antibiotic.
In terms of common clinical uses, cephalosporins are frequently employed in the treatment of community-acquired and nosocomial pneumonia, skin and soft tissue infections, urinary tract infections, and meningitis. Fluoroquinolones, on the other hand, are widely used for the management of respiratory tract infections, urinary tract infections, gastrointestinal infections, and sexually transmitted diseases, as well as chronic prostatitis and osteomyelitis.
Regarding potential side effects, both antibiotic classes have been associated with a range of adverse events. Cephalosporins have been known to cause allergic reactions, gastrointestinal disturbances, and, in rare cases, nephrotoxicity. Fluoroquinolones, meanwhile, have been linked to an increased risk of tendinitis, tendon rupture, peripheral neuropathy, and central nervous system effects, such as headaches and dizziness. Healthcare providers must carefully weigh the benefits and risks when prescribing these antibiotics, particularly in vulnerable populations.
As the scientific community continues to explore new strategies to combat antimicrobial resistance, the ongoing comparison of cephalosporins and fluoroquinolones remains a crucial component of the broader effort to optimize antibiotic usage and improve patient outcomes. What are your thoughts on the relative merits and drawbacks of these two important antibiotic classes? Share your insights and experiences to further the dialogue on this important topic.
User comments
More Topics to Explore
What Are the Common Side Effects of Cephalosporins?
This thread discusses the common side effects associated with the use of cephalosporins, a widely used class of antibiotics, inviting members to share their experiences and insights.
Can Cephalosporins Be Used Safely During Pregnancy?
Join this thread to discuss the safety of using cephalosporins during pregnancy, sharing any guidelines, research, or personal experiences related to this topic.
What Makes Cephalosporins Different from Penicillin?
Engage in this thread to explore the key differences between cephalosporins and penicillin in terms of their chemical structures, mechanisms of action, and spectrum of activity.
Are Cephalosporins Effective Against MRSA Infections?
Dive into this thread to examine the effectiveness of cephalosporins in treating MRSA (Methicillin-resistant Staphylococcus aureus) infections, sharing any relevant research findings or clinical experiences.
What Precautions Should Be Taken When Administering Cephalosporins to Children?
Participate in this thread to share best practices and precautions to ensure safe administration of cephalosporins in pediatric patients, promoting a collaborative exchange of insights among members.
Can Cephalosporins Cause Allergic Reactions?
Explore the potential for cephalosporins to induce allergic reactions in patients, discussing risk factors, symptoms, and management strategies for cephalosporin allergies to enhance member awareness.
What Are the Guidelines for Switching Patients from Penicillin to Cephalosporins?
Engage in this conversation to discuss the recommended guidelines and considerations when transitioning patients from penicillin to cephalosporins, highlighting key factors that healthcare providers should keep in mind.
Do Cephalosporins Interact with Other Medications?
Join this thread to explore potential drug interactions involving cephalosporins, sharing information on common medications that may interact with cephalosporins and discussing strategies to mitigate these interactions.
What Are the Emerging Trends in Cephalosporin Development?
Delve into this thread to discover the latest advancements and emerging trends in the development of cephalosporins as a crucial class of antibiotics, exchanging knowledge on new formulations, mechanisms of action, and resistance patterns.