How does antibiotic resistance impact vulnerable populations?
Examine the disproportionate effects of antibiotic resistance on vulnerable communities and individuals with limited access to healthcare.
How Antibiotic Resistance Affects the Most Vulnerable
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Apr-09
Antibiotic resistance is a pressing global health concern, with far-reaching consequences for communities around the world. However, the impact of this crisis is not felt equally – vulnerable populations, including those with limited access to healthcare, often bear the brunt of this growing problem.
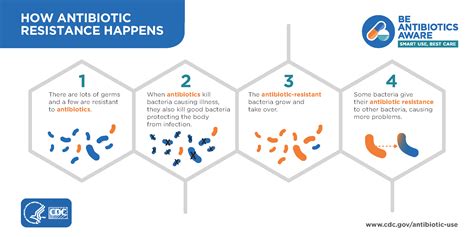
At the heart of the issue lies the inherent nature of antibiotic resistance. As bacteria evolve to withstand the effects of antimicrobial drugs, certain infections become increasingly difficult to treat. This phenomenon is exacerbated by the overuse and misuse of antibiotics, a practice that is more prevalent in areas with inadequate healthcare infrastructure.
Vulnerable populations, such as the elderly, children, and individuals with compromised immune systems, are particularly susceptible to the dangers of antibiotic-resistant infections. These individuals may have weaker immune responses, making them more prone to contracting severe, hard-to-treat illnesses. Moreover, their limited access to quality medical care can delay diagnosis and appropriate treatment, further exacerbating the situation.
In many developing countries, the lack of access to essential medicines, including effective antibiotics, is a significant contributor to the disproportionate impact of antibiotic resistance. Poverty, limited healthcare funding, and substandard sanitation conditions all contribute to the spread of resistant bacteria, as individuals may lack the resources to obtain or properly administer the necessary medications.
The consequences of antibiotic resistance for vulnerable populations can be devastating. Infections that were once easily treatable may now require prolonged hospital stays, more expensive and complex treatments, and an increased risk of complications or even death. This places an enormous burden on individuals, families, and healthcare systems, perpetuating the cycle of inequality and limiting access to essential care.
To address this complex issue, a multifaceted approach is required. Improving access to quality healthcare, promoting the responsible use of antibiotics, and investing in the development of new antimicrobial agents are all crucial steps in mitigating the impact of antibiotic resistance on vulnerable populations.
Public health initiatives that focus on education, infection control, and the strengthening of healthcare infrastructure can help empower communities and reduce the spread of resistant bacteria. Additionally, international collaborations and policies that prioritize equitable access to essential medicines can play a vital role in ensuring that vulnerable populations are not left behind in the fight against antibiotic resistance.
As we strive to tackle this global challenge, it is essential to recognize the disproportionate burden borne by the most vulnerable members of our society. By addressing the root causes and implementing targeted interventions, we can work towards a future where antibiotic resistance no longer poses a threat to those who need our support the most.
What other strategies can be implemented to protect vulnerable populations from the devastating effects of antibiotic resistance?
User comments
More Topics to Explore
Why do bacteria develop antibiotic resistance?
Discuss the reasons behind the development of antibiotic resistance in bacteria and its implications for healthcare.
How can we combat antibiotic resistance?
Share strategies and methods to tackle the growing issue of antibiotic resistance in healthcare settings.
What are the consequences of antibiotic misuse?
Delve into the harmful effects of improper antibiotic use on individual health and global antibiotic resistance.
Is antibiotic resistance a global health threat?
Debate the extent to which antibiotic resistance poses a significant risk to global health and healthcare systems.
Are there natural alternatives to antibiotics?
Share insights on natural remedies that can potentially provide alternatives to traditional antibiotics in treating bacterial infections.
How do antibiotics contribute to antibiotic resistance?
Examine the relationship between antibiotic use and the development of antibiotic resistance in microbial populations.
What role do healthcare providers play in combating antibiotic resistance?
Highlight the essential role that healthcare professionals play in fighting antibiotic resistance through responsible prescribing practices.
Could bacteriophages be the solution to antibiotic resistance?
Discuss the potential of bacteriophages as an alternative therapy in fighting antibiotic-resistant bacterial infections.
What are the economic implications of antibiotic resistance?
Explore the economic consequences of antibiotic resistance on healthcare systems, including increased treatment costs and productivity losses.