Navigating the Complex Landscape of Antiviral and Antibiotic Resistance
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-27
As the world grapples with the ever-evolving threat of infectious diseases, understanding the nuances between antiviral resistance and antibiotic resistance has become increasingly crucial. While both phenomena pose significant challenges to healthcare professionals and public health authorities, the underlying mechanisms and their implications can vary significantly.
At the core of this distinction lies the fundamental difference between viruses and bacteria. Viruses are non-living entities that rely on host cells to replicate and propagate, whereas bacteria are living, independent organisms. This distinction is paramount when it comes to the development of resistance.
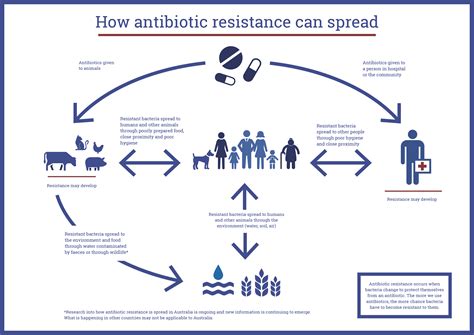
Antibiotic resistance typically arises from genetic mutations or the acquisition of resistance genes that allow bacteria to survive and thrive in the presence of antibiotic drugs. These adaptations can render once-effective antibiotics powerless, leading to the emergence of superbugs – strains of bacteria that are resistant to multiple or even all available antibiotics. The consequences of antibiotic resistance can be severe, as it hampers our ability to treat common infections and increases the risk of complications, prolonged illness, and even death.
In contrast, antiviral resistance often manifests differently. Viruses, being non-living, do not possess the same mechanisms for genetic adaptation as bacteria. Instead, antiviral resistance can develop through mutations that allow the virus to evade the effects of antiviral drugs or to replicate more efficiently in the presence of these medications. This can be particularly problematic for chronic viral infections, such as HIV or hepatitis C, where the virus may accumulate mutations over time, rendering once-effective treatments less potent.
Furthermore, the impact of antiviral resistance can vary depending on the specific virus and the available treatment options. For some viruses, like influenza, the development of resistance may be more common and can affect the effectiveness of seasonal vaccines and antiviral medications. For other viruses, such as the SARS-CoV-2 virus that causes COVID-19, the emergence of resistance has been less prevalent, at least in the early stages of the pandemic.
The challenges in addressing antiviral and antibiotic resistance are multifaceted. In the case of antibiotics, the development of new drugs has slowed in recent decades, while the overuse and misuse of these medications have accelerated the spread of resistance. For antivirals, the fast-paced evolution of viruses, combined with the limited arsenal of effective treatments, can make it difficult to stay ahead of the curve.
To combat these threats, a comprehensive approach is required, involving improved surveillance, responsible antibiotic and antiviral stewardship, accelerated research and development of new therapeutic options, and enhanced public education. By understanding the nuances between antiviral and antibiotic resistance, healthcare providers and policymakers can devise more targeted strategies to address these pressing public health challenges and safeguard the well-being of individuals and communities worldwide.
As we continue to navigate the complex landscape of infectious disease management, the ability to distinguish between antiviral and antibiotic resistance will be crucial in shaping our response and ensuring the long-term effectiveness of our medical interventions. What other insights can you offer on this critical topic?