When Antibiotics and Antivirals Join Forces: The Importance of Patient Education
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Apr-12
The advent of combination therapy, where antibiotics and antivirals are prescribed together, has revolutionized the treatment of complex infections. This approach aims to tackle the underlying pathogen from multiple angles, enhancing the efficacy of the treatment. However, the successful implementation of this strategy relies heavily on educating the patient and ensuring their active participation in the care process.
At the core of combination therapy is the need for patients to understand the rationale behind the prescribed regimen. Antibiotics are designed to target bacterial infections, while antivirals are tailored for viral diseases. By combining these two classes of medications, healthcare providers can address the potential presence of both bacterial and viral components in a patient's condition. This comprehensive approach can lead to improved outcomes, but it also requires the patient to navigate a more complex treatment plan.
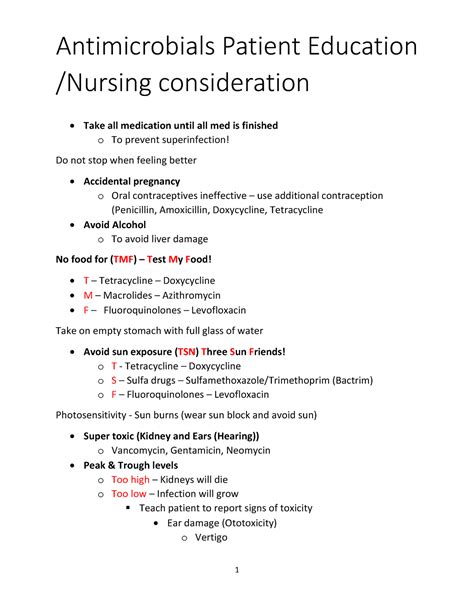
Effective patient education begins with clear communication of the treatment objectives. Patients should be made aware of the specific infections they are facing, the rationale for the chosen combination therapy, and the anticipated timeline for recovery. Incorporating visual aids, such as diagrams or infographics, can further enhance the patient's understanding of the underlying mechanisms at play.
Adherence to the prescribed medication regimen is crucial for the success of combination therapy. Patients must be educated on the importance of taking the medications as directed, including the specific dosing schedules, timing, and any potential interactions with food or other medications. Reinforcing the need for consistent and diligent administration can help prevent suboptimal outcomes and the development of antibiotic resistance or antiviral resistance.
Equally important is the discussion of potential side effects associated with the combined use of antibiotics and antivirals. Patients should be informed about the common side effects, such as gastrointestinal disturbances, skin reactions, or changes in liver function, and be empowered to report any concerning symptoms promptly. Equipping patients with strategies to manage these side effects, such as dietary modifications or the use of probiotics, can enhance their comfort and overall adherence to the treatment plan.
Furthermore, patient education should address the importance of completing the entire course of combination therapy, even if symptoms improve before the recommended duration. Emphasizing the need to adhere to the full treatment regimen can help prevent the resurgence of infections or the emergence of drug-resistant strains.
By effectively communicating the rationale, adherence requirements, and potential side effects of combination therapy, healthcare providers can empower patients to play an active role in their treatment journey. This collaborative approach not only enhances the chances of successful outcomes but also fosters a sense of trust and partnership between the patient and the healthcare team.
As we navigate the evolving landscape of infectious disease management, the role of patient education in combination therapy cannot be overstated. By equipping patients with the necessary knowledge and tools, we can pave the way for improved treatment adherence, clinical outcomes, and ultimately, better overall patient health.
What strategies have you found most effective in educating patients about the complexities of antibiotics and antivirals combination therapy? Share your insights and experiences in the comments below.