Antiviral resistance is a growing concern in the medical community as it poses significant challenges in effectively managing and treating viral infections. The development of antiviral resistance is a complex phenomenon influenced by various factors, both biological and behavioral. Let's delve into the key factors that contribute to the emergence and spread of this critical issue.
Viral Mutation and Adaptation
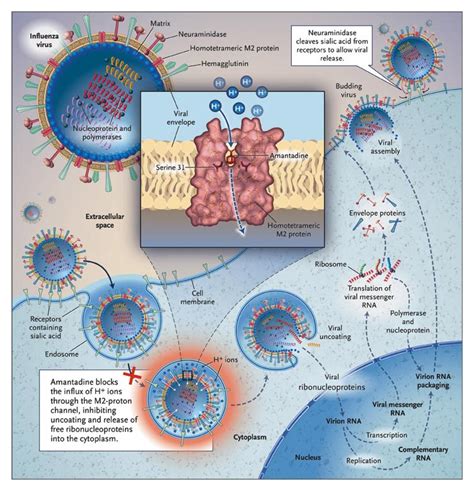
At the heart of antiviral resistance lies the remarkable ability of viruses to mutate and adapt. Viruses, being simple organisms, possess a high rate of genetic replication and a propensity for errors during the replication process. This creates a diverse population of viral variants, some of which may exhibit resistance to specific antiviral drugs. As these resistant strains proliferate, they can become the dominant form, rendering the original treatment ineffective.
Incomplete Viral Clearance
Incomplete viral clearance, often due to premature cessation of treatment or suboptimal drug dosing, can contribute to the development of antiviral resistance. When the viral load is not sufficiently reduced, it provides an environment for the selection and amplification of resistant viral variants, as they have the opportunity to continue replicating and spreading.
Widespread and Indiscriminate Use of Antivirals
The widespread and sometimes indiscriminate use of antiviral medications, particularly in the absence of proper diagnosis or clinical guidelines, can exacerbate the problem of antiviral resistance. Overuse or inappropriate use of these drugs can create selective pressure, favoring the survival and propagation of resistant viral strains.
Lack of Adherence to Treatment Regimens
Poor adherence to prescribed antiviral treatment regimens, such as missed doses or early discontinuation of therapy, can also contribute to the development of resistance. Inconsistent drug levels in the body can allow the virus to adapt and develop resistance mechanisms.
Cross-Resistance and Co-Resistance
The phenomenon of cross-resistance, where a virus becomes resistant to multiple antiviral drugs with similar mechanisms of action, can further complicate the treatment landscape. Additionally, co-resistance, where a virus develops resistance to multiple unrelated antiviral agents, can severely limit the available treatment options for healthcare providers.
Viral Reservoirs and Latency
The existence of viral reservoirs, where the virus can persist in a latent or dormant state, poses a significant challenge. These reservoirs can serve as a source for the reactivation and spread of resistant viral strains, even in the presence of effective antiviral therapy.
Genetic Diversity and Reassortment
Certain viruses, such as influenza, possess a high degree of genetic diversity and the ability to undergo genetic reassortment, where different viral strains exchange genetic material. This can lead to the emergence of novel, resistant viral variants that may be more challenging to combat.
Lack of Novel Antiviral Drugs
The limited development of new and innovative antiviral drugs, particularly in the face of rapidly evolving viral resistance, can hinder the ability to effectively manage and control resistant infections.
As we continue to grapple with the complexities of antiviral resistance, it is crucial that healthcare professionals, researchers, and policymakers work collaboratively to address these multifaceted challenges. Strategies such as improved diagnostic tools, optimized treatment regimens, enhanced surveillance, and the development of novel antiviral agents will be essential in the ongoing fight against the growing threat of antiviral resistance.
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-18