Combating Antiviral Resistance in HIV Care: The Necessity of Collaborative Efforts
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Apr-12
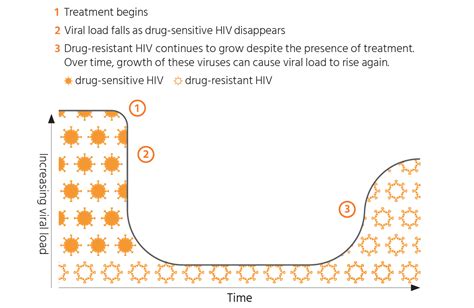
The management of HIV has seen remarkable advancements in recent decades, with the development of antiretroviral therapies (ARTs) that have transformed the lives of millions living with the virus. However, the constant evolution of HIV and the emergence of antiviral resistance pose a significant challenge to maintaining the effectiveness of these life-saving treatments. Addressing this issue requires a collaborative approach involving various stakeholders, including healthcare providers, researchers, policymakers, and community organizations.
At the forefront of this challenge are healthcare providers, who play a vital role in monitoring and managing antiviral resistance in their patients. By closely monitoring patient responses to ARTs and promptly identifying signs of resistance, they can make informed decisions about changing treatment regimens or implementing alternative strategies. Moreover, healthcare providers can contribute to research efforts by sharing data and insights from their clinical experiences, ultimately informing the development of more effective and tailored interventions.
Researchers, on the other hand, are essential in advancing our understanding of the mechanisms underlying antiviral resistance and exploring innovative solutions. Through laboratory investigations, epidemiological studies, and clinical trials, they can uncover the genetic and molecular factors that drive resistance, as well as develop new classes of antiretroviral drugs, novel delivery methods, and personalized treatment approaches. By fostering collaboration between researchers from diverse fields, such as virology, pharmacology, and immunology, a more comprehensive understanding of the resistance challenge can be achieved.
Policymakers play a crucial role in creating an enabling environment for addressing antiviral resistance in HIV care. They can develop and implement policies that ensure access to a diverse range of antiretroviral drugs, promote the rational use of medications, and support the monitoring and surveillance of resistance patterns. Additionally, policymakers can facilitate the allocation of resources for research and development, as well as the implementation of comprehensive treatment and prevention programs that integrate resistance management strategies.
Community organizations, often serving as the link between healthcare systems and the individuals affected by HIV, can contribute significantly to the collaborative effort. By engaging with people living with HIV, these organizations can gather valuable insights into the real-world challenges faced by patients, including adherence barriers, access to care, and the sociocultural factors that influence treatment outcomes. This information can then be shared with healthcare providers and policymakers, informing the design of more patient-centered and responsive strategies to address antiviral resistance.
Fostering effective collaboration among these diverse stakeholders is essential in combating the challenge of antiviral resistance in HIV care. By aligning their efforts, sharing knowledge and resources, and coordinating their strategies, healthcare providers, researchers, policymakers, and community organizations can collectively develop a comprehensive approach that addresses the multifaceted nature of this issue. Through such collaborative efforts, the goal of ensuring sustainable and effective HIV management can be more readily achieved, ultimately improving the lives of those affected by the virus.
What other key stakeholders or innovative approaches do you believe should be involved in the collaborative effort to address antiviral resistance in HIV care?