The Troubling Impact of Antibiotic and Antiviral Misuse on Combination Therapy
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Apr-09
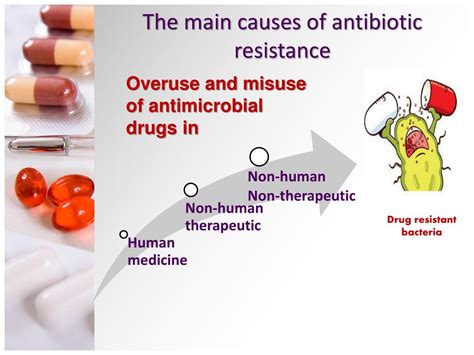
As the medical community grapples with the rising tide of antibiotic resistance, the use of combination therapy has become increasingly crucial for tackling complex infections. However, the widespread misuse and overuse of both antibiotics and antivirals threaten to undermine the very foundation of this critical treatment approach.
The emergence of multidrug-resistant pathogens, fueled by irresponsible prescription practices and patient noncompliance, has forced clinicians to rely more heavily on combination therapy. By utilizing two or more antimicrobial agents simultaneously, the goal is to enhance the antimicrobial activity, prevent the development of resistance, and ultimately improve patient outcomes. This strategy has proven particularly effective against infections caused by bacteria, viruses, and even fungi that have developed resistance to individual drugs.
Yet, the very same factors that have necessitated the rise of combination therapy – the misuse of antibiotics and antivirals – also threaten to compromise its effectiveness. Inappropriate drug selection, suboptimal dosing, and failure to adhere to prescribed treatment regimens can all contribute to the problem, leading to therapeutic failure and the further propagation of resistant strains.
One of the primary concerns surrounding the misuse of these medications is the increased risk of drug interactions. When multiple antimicrobial agents are used concurrently, they can potentially interfere with each other's metabolism, absorption, or mechanism of action, resulting in reduced therapeutic efficacy or even heightened toxicity. This delicate balance must be carefully monitored and managed by healthcare providers, lest the combination therapy becomes more detrimental than beneficial.
Moreover, the practice of suboptimal dosing, whether intentional or unintentional, can also undermine the effectiveness of combination therapy. Inadequate drug concentrations may fail to eradicate the targeted pathogens, allowing them to persist and potentially develop resistance. Conversely, excessively high doses can increase the risk of adverse effects and drug interactions, further complicating the treatment process.
The implications of these issues extend far beyond the individual patient, as the emergence and spread of antibiotic-resistant and antiviral-resistant strains can have far-reaching public health consequences. These resistant microbes can be transmitted to others, leading to outbreaks and epidemics that are increasingly difficult to manage.
To address this critical challenge, a multifaceted approach is required. healthcare providers must exercise prudence in prescribing antibiotics and antivirals, ensuring that they are only used when necessary and in accordance with evidence-based guidelines. Patients, on the other hand, must be educated on the importance of completing prescribed treatment regimens and following dosing instructions meticulously.
Additionally, regulatory bodies and policymakers have a crucial role to play in developing and enforcing stricter guidelines for the use of these crucial medications, as well as investing in the development of novel antimicrobial agents to combat the ever-evolving threats posed by resistant pathogens.
As the battle against complex infections continues, the responsible and judicious use of antibiotics and antivirals will be paramount in preserving the effectiveness of combination therapy and safeguarding the health of individuals and communities worldwide. The stakes have never been higher, and the time for action is now.