What role do culture and sensitivity testing play in guiding antibiotic therapy in pediatric patients?
Explore the significance of culture and sensitivity testing in tailoring antibiotic therapy for pediatric patients. Discuss the impact of accurate microbial identification on treatment outcomes, antibiotic selection, and combating antimicrobial resistance in pediatric populations.
Culture and Sensitivity Testing: A Critical Component in Pediatric Antibiotic Therapy
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Apr-12
As parents, we strive to provide the best possible care for our children, especially when they are faced with infections that require antibiotic treatment. In the realm of pediatric medicine, the role of culture and sensitivity testing cannot be overstated. These diagnostic tools play a crucial part in guiding the selection of appropriate antibiotics and ensuring favorable treatment outcomes for our young patients.
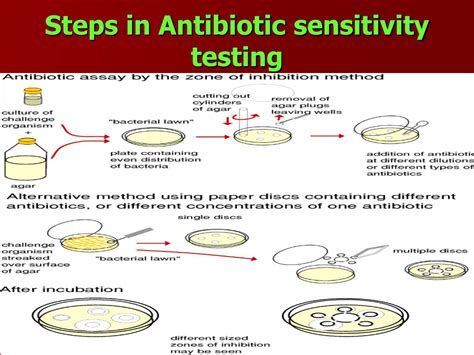
The identification of the causative pathogen is the cornerstone of effective antibiotic therapy. Accurate microbial identification through culture and sensitivity testing allows healthcare professionals to tailor the treatment plan to the specific needs of the child. By determining the susceptibility of the infecting organism to various antibiotics, clinicians can make informed decisions about the most appropriate drug and dosage, minimizing the risk of treatment failure and the development of antimicrobial resistance.
In the context of pediatric patients, this level of precision is especially important. Children's immune systems are still developing, and they may be more vulnerable to complications from infections. The choice of antibiotic can significantly impact the course of the illness, the child's recovery, and the long-term health implications. By relying on culture and sensitivity testing, healthcare providers can ensure that the selected antibiotic effectively targets the causative pathogen while minimizing the risk of adverse effects and the potential for the emergence of resistant strains.
Moreover, the judicious use of antibiotics is crucial in the pediatric population. Overuse or inappropriate use of these medications can lead to the development of antibiotic-resistant bacteria, which can have far-reaching consequences. Culture and sensitivity testing helps healthcare providers make informed decisions about antibiotic selection, promoting the responsible use of these vital drugs and contributing to the global effort to combat antimicrobial resistance.
In addition to its role in guiding initial antibiotic selection, culture and sensitivity testing also plays a crucial part in monitoring the effectiveness of treatment. If a child's condition does not improve as expected, or if the infection recurs, further testing can provide valuable insights into the causative pathogen and its response to the prescribed antibiotics. This information allows healthcare providers to make necessary adjustments to the treatment plan, ensuring the best possible outcome for the child.
As parents, we may feel anxious when our children require antibiotic therapy. However, by understanding the importance of culture and sensitivity testing in the pediatric setting, we can take comfort in the knowledge that our healthcare providers are equipped with the necessary tools to make informed decisions and provide the most appropriate care for our little ones.
In conclusion, the role of culture and sensitivity testing in guiding antibiotic therapy for pediatric patients is undeniably crucial. By accurately identifying the causative pathogen and its susceptibility to various antibiotics, healthcare providers can tailor the treatment plan to the individual needs of the child, promote the responsible use of these vital medications, and work towards combating the global challenge of antimicrobial resistance. As parents, we can take an active role in understanding and advocating for the importance of these diagnostic tools, ensuring the best possible outcomes for our children's health.
User comments
More Topics to Explore
Is it necessary to strictly adhere to pediatric antibiotic prescribing guidelines?
Explore the importance of adhering to pediatric antibiotic prescribing guidelines and discuss the potential consequences of non-compliance. Share your insights and experiences on this topic.
What are the key considerations when prescribing antibiotics to pediatric patients?
Delve into the essential factors to consider when prescribing antibiotics to pediatric patients. Share your knowledge on dosage adjustments, age-specific recommendations, and potential side effects in the pediatric population.
How do pediatric antibiotic prescribing guidelines differ from adult guidelines?
Discuss the unique aspects of pediatric antibiotic prescribing guidelines compared to adult guidelines. Explore the reasons behind these differences and their impact on clinical practice. Share any challenges or successes you have encountered when navigating these distinctions.
What role do pediatric antibiotic prescribing guidelines play in antimicrobial stewardship?
Investigate the contributions of pediatric antibiotic prescribing guidelines to antimicrobial stewardship efforts. Share strategies for promoting responsible antibiotic use in the pediatric setting and discuss the implications for long-term antibiotic resistance.
Are there any challenges in implementing pediatric antibiotic prescribing guidelines in clinical practice?
Explore the obstacles that healthcare providers face when implementing pediatric antibiotic prescribing guidelines in real-world clinical settings. Share tips for overcoming these challenges and optimizing adherence to guidelines.
What resources are available to support healthcare providers in following pediatric antibiotic prescribing guidelines?
Share valuable resources and tools that can assist healthcare providers in adhering to pediatric antibiotic prescribing guidelines. Discuss the role of clinical decision support systems, guidelines publications, and professional organizations in supporting pediatric antibiotic stewardship.
How do pediatric antibiotic prescribing guidelines impact the management of common childhood infections?
Examine the influence of pediatric antibiotic prescribing guidelines on the treatment of prevalent childhood infections. Discuss specific recommendations for conditions such as otitis media, pharyngitis, and pneumonia, and share insights on optimizing antibiotic therapy in these cases.
What factors should be considered when selecting the most appropriate antibiotic for pediatric patients?
Delve into the key factors that healthcare providers should consider when choosing the most suitable antibiotic for pediatric patients. Discuss considerations such as microbiological data, safety profiles, dosing schedules, and patient-specific factors influencing antibiotic selection.
How can healthcare providers ensure patient and caregiver understanding of pediatric antibiotic prescribing guidelines?
Share strategies for effectively communicating pediatric antibiotic prescribing guidelines to patients and caregivers. Discuss the importance of patient education in promoting adherence to treatment plans, enhancing antibiotic stewardship practices, and preventing antibiotic misuse.