Abdominal Infections: Types and Treatment
Abdominal Infections FAQ
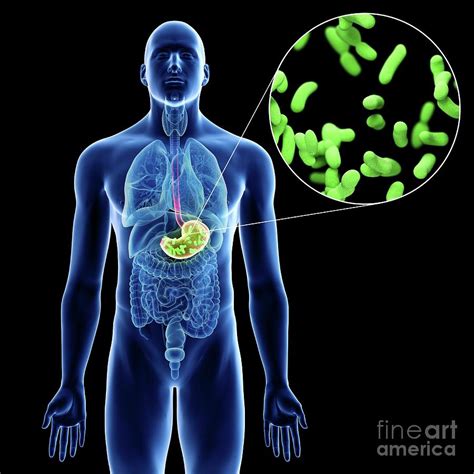
What germs can cause a stomach infection?
Different germs—bacteria, parasites, and viruses—can all lead to stomach infections. The germs responsible for abdominal infections can depend on: Abdominal infections can also be differentiated by where you initially get infected. Community-acquired infections are spread outside of healthcare facilities, such as hospitals.
What is a bowel infection called?
The gut (also called bowel or intestine), is part of your digestive system. An infection of the bowel is sometimes called a gastrointestinal infection, or gastroenteritis or (gastro). You can get gastroenteritis by eating or drinking contaminated water or food. This is often called food poisoning)
What is a common bacterial gastrointestinal infection?
Common bacterial gastrointestinal infections include: Campylobacter. Clostridioides difficile (C. diff). Escherichia coli (E. coli). Salmonella. Shigella. Staphylococci (Staph). Parasite infections cause parasitic gastroenteritis. Common parasite infections include: Giardiasis. Cryptosporidiosis. Cyclosporiasis. Amebiasis (amoebic dysentery).
What causes infection in the abdominal cavity?
Literature review current through: Feb 2024. This topic last updated: Dec 01, 2023. Infections within the abdominal cavity typically arise because of inflammation or disruption of the gastrointestinal tract. Less commonly, they can arise from the gynecologic or urinary tract.
What is the pathophysiology of intra-abdominal infections in adults?
Abdominal infections are usually polymicrobial and result in an intra-abdominal abscess or secondary peritonitis, which may be generalized or localized (phlegmon). The approach to antimicrobial selection and administration for intra-abdominal infections in adults is discussed here.
What causes intra-abdominal infections?
Intra-abdominal infections usually arise after a breach in the intrinsic mucosal defense barrier that allows normal bowel flora to inoculate the abdominal cavity. The precise microbiological spectrum depends on the precise gastrointestinal source (ie, small versus large bowel).
Abdominal Infections References
If you want to know more about Abdominal Infections, consider exploring links below:
What Is Abdominal Infections
- https://www.healthdirect.gov.au/bowel-infections
- https://www.medicalnewstoday.com/articles/gastrointestinal-infection
- https://www.healthline.com/health/gastrointestinal-infection
- https://www.mayoclinic.org/diseases-conditions/viral-gastroenteritis/symptoms-causes/syc-20378847
- https://www.health.com/condition/gastrointestinal-infections-overview
- https://my.clevelandclinic.org/health/diseases/gastroenteritis
- https://www.verywellhealth.com/bacterial-gastroenteritis-5219755
Abdominal Infections Information
Explore Related Topics
How can genetic testing support public health efforts to combat antibiotic resistance?
Explore the role of genetic testing in surveillance, outbreak investigations, and public health interventions aimed at controlling the spread of antibiotic-resistant pathogens. Share your perspectives on the potential impact of genetic testing on population health and antimicrobial stewardship initiatives.
How Do Cephalosporins Compare to Fluoroquinolones as Antibiotics?
Join this discussion to compare and contrast cephalosporins and fluoroquinolones in terms of their spectrum of activity, common uses, and potential side effects, fostering an exchange of knowledge among members.
What are the Risks of Overusing Antibiotics in Patients?
Join the discussion on the potential dangers and risks associated with the overuse of antibiotics in patients. How can healthcare providers effectively communicate the risks to patients to promote responsible antibiotic use?
What are the challenges in managing drug-resistant infections?
Delve into the complexities and hurdles faced in managing drug-resistant infections, discussing the various challenges healthcare professionals encounter in treating such cases.