Are macrolides a suitable choice for patients with penicillin allergies?
Discuss the suitability of prescribing macrolide antibiotics to patients allergic to penicillin. Share any guidelines or precautions when considering macrolides as an alternative in penicillin-allergic individuals.
Macrolides: A Potential Lifeline for Penicillin-Allergic Patients
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-24
The world of medicine is often a delicate balance between efficacy and safety, and this rings particularly true when it comes to the treatment of infections. For patients with a known allergy to penicillin, a common and highly effective class of antibiotics, the task of finding a suitable alternative becomes a critical consideration for healthcare providers. Enter the macrolides – a family of antibiotics that may offer a viable solution for those individuals intolerant to penicillin.
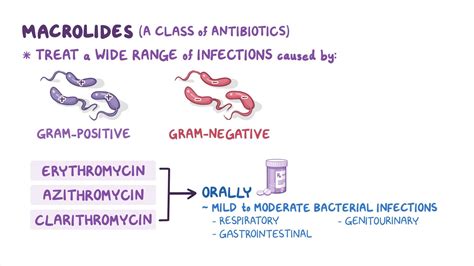
Macrolides are a group of antibiotics that share a common chemical structure, including erythromycin, clarithromycin, and azithromycin. These medications have long been recognized for their broad-spectrum antimicrobial activity, making them a go-to choice for a variety of bacterial infections. But for penicillin-allergic patients, macrolides may hold an even greater significance.
Studies have shown that the risk of cross-reactivity between penicillin and macrolides is relatively low, typically ranging from 5 to 10 percent. This means that the majority of individuals with a penicillin allergy can safely utilize macrolide antibiotics without fear of triggering a similar adverse reaction.
However, it's important to note that the decision to prescribe macrolides for penicillin-allergic patients should not be taken lightly. Healthcare providers must carefully evaluate the patient's medical history, severity of the penicillin allergy, and the specific infection being treated. In some cases, the use of macrolides may be contraindicated or require additional precautions.
1. Allergy Evaluation: Patients with a history of penicillin allergy should undergo proper allergy testing to confirm the specific nature and severity of their reaction. This information can help guide the appropriate antibiotic selection.
2. Antibiotic Stewardship: Macrolides should be used judiciously, as overuse can contribute to the development of antibiotic resistance. Healthcare providers should carefully weigh the risks and benefits of macrolide therapy for each individual patient.
3. Monitoring for Adverse Events: Patients receiving macrolide antibiotics should be closely monitored for any signs of adverse reactions, such as gastrointestinal disturbances, liver dysfunction, or allergic responses.
By adhering to these guidelines and exercising caution, healthcare providers can potentially offer macrolides as a suitable alternative for penicillin-allergic patients, providing them with effective treatment options and reducing the risk of potentially life-threatening reactions.
As the medical community continues to navigate the complexities of antibiotic selection and allergy management, the role of macrolides in the treatment of penicillin-allergic individuals remains a topic of ongoing research and clinical evaluation. The careful and judicious use of these antibiotics may just be the key to unlocking a safer and more effective path forward for those individuals who have found themselves at the mercy of a penicillin allergy.
What are your thoughts on the use of macrolides for penicillin-allergic patients? Have you or a loved one experienced the challenges of finding suitable antibiotic alternatives? Share your insights and experiences in the comments below.
User comments
More Topics to Explore
Are macrolides safe for pregnant women?
Discuss the safety of using macrolide antibiotics during pregnancy, considering potential benefits and risks for both the mother and the baby. Share any relevant studies or guidelines on this topic.
Can macrolides be used to treat respiratory infections in children?
Share experiences or recommendations regarding the use of macrolide antibiotics in treating respiratory infections in children. Discuss any considerations or precautions that should be taken when using macrolides in pediatric patients.
What are the common side effects of macrolide antibiotics?
Explore and list the common side effects and adverse reactions associated with macrolide antibiotics. Share personal experiences or precautions to manage these side effects effectively.
Do macrolides interact with common medications?
Explore potential drug interactions between macrolide antibiotics and commonly used medications. Share any precautions or recommendations for patients who are taking macrolides along with other drugs.
Are macrolides effective in treating atypical pneumonia?
Discuss the efficacy of macrolide antibiotics in treating atypical pneumonia. Share any clinical experiences, studies, or guidelines supporting the use of macrolides for this specific type of respiratory infection.
Can prolonged use of macrolides lead to antibiotic resistance?
Explore the potential risk of antibiotic resistance associated with prolonged use of macrolide antibiotics. Discuss strategies to mitigate resistance development while using macrolides for long-term treatment.
What are the key differences between macrolides and other classes of antibiotics?
Compare and contrast macrolide antibiotics with other classes of antibiotics in terms of mechanism of action, spectrum of activity, common uses, and potential side effects. Share any unique characteristics that set macrolides apart from other antibiotic categories.
Are there any dietary restrictions when taking macrolide antibiotics?
Discuss if there are any specific dietary restrictions or considerations that patients should be aware of when taking macrolide antibiotics. Share any information on potential interactions between certain foods and macrolides.
How do macrolides compare to fluoroquinolones in treating respiratory infections?
Compare and contrast the efficacy and safety of macrolide antibiotics versus fluoroquinolones in the treatment of respiratory infections. Discuss any factors that influence the choice between these two classes of antibiotics for respiratory tract infections.