Can prolonged use of macrolides lead to antibiotic resistance?
Explore the potential risk of antibiotic resistance associated with prolonged use of macrolide antibiotics. Discuss strategies to mitigate resistance development while using macrolides for long-term treatment.
The Rise of Macrolide Resistance: A Cautionary Tale
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Apr-02
As the medical community continues to grapple with the alarming spread of antibiotic resistance, one class of drugs that has come under increased scrutiny is the macrolides. These widely-used antimicrobial agents, which include medications like erythromycin, clarithromycin, and azithromycin, have long been a mainstay in the treatment of a variety of bacterial infections. However, growing evidence suggests that the prolonged or inappropriate use of macrolides may be contributing to the very problem they were intended to solve - the emergence of drug-resistant bacteria.
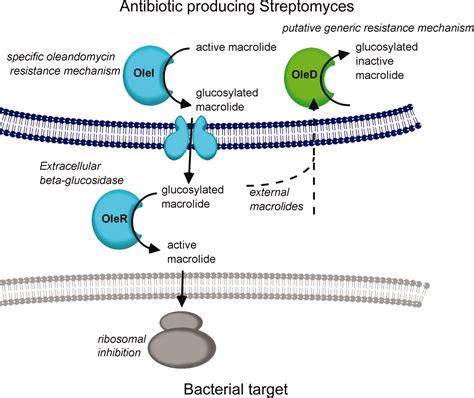
The concern over macrolide resistance stems from the drugs' mechanism of action and their widespread application. Macrolides work by interfering with the protein synthesis machinery of bacteria, effectively inhibiting their ability to replicate and spread. While this makes them effective against a range of pathogens, it also means that bacteria have had ample opportunity to evolve countermeasures over time. As macrolides have been extensively prescribed for conditions ranging from respiratory tract infections to skin and soft tissue infections, the selective pressure has been immense, favoring the survival and proliferation of resistant strains.
Studies have shown that prolonged or repeated courses of macrolide therapy can significantly increase the risk of macrolide-resistant infections. This is particularly problematic in conditions that require long-term management, such as chronic obstructive pulmonary disease (COPD) or cystic fibrosis, where macrolides are often used as maintenance therapies. In these scenarios, the sustained exposure to the drugs can create a breeding ground for resistant bacteria, rendering the medications less effective over time.
Moreover, the problem of macrolide resistance is not limited to the specific drugs within this class. Due to the structural similarities and shared mechanisms of action, resistance to one macrolide can confer cross-resistance to others, further limiting treatment options for patients. This creates a concerning scenario where the very antibiotics meant to treat infections may ultimately contribute to the development of even more formidable, multidrug-resistant pathogens.
To address this challenge, healthcare providers and policymakers have been actively exploring strategies to mitigate the risk of antibiotic resistance associated with macrolide use. One approach is the judicious and appropriate prescribing of these drugs, ensuring that they are only used when truly necessary and for the shortest duration possible. This can involve the implementation of antimicrobial stewardship programs that provide guidance on the optimal use of macrolides and other antibiotics.
Additionally, researchers are investigating alternative treatment approaches that may reduce the reliance on macrolides. This includes the exploration of novel antimicrobial agents, the development of diagnostic tools to better target specific pathogens, and the incorporation of non-antibiotic therapies, such as immunomodulatory treatments, into patient management plans.
As the battle against antibiotic resistance continues, the role of macrolides in clinical practice remains a delicate balance. While these medications have undoubtedly saved countless lives, their prolonged use carries the risk of fueling the very problem they were meant to solve. By employing a multifaceted approach that prioritizes responsible antibiotic stewardship, healthcare professionals can work to mitigate the rise of macrolide resistance and ensure that these vital drugs remain effective for generations to come.
What are your thoughts on the challenges posed by macrolide resistance, and how can we best address this issue to protect public health? Share your insights in the comments below.
User comments
More Topics to Explore
Are macrolides safe for pregnant women?
Discuss the safety of using macrolide antibiotics during pregnancy, considering potential benefits and risks for both the mother and the baby. Share any relevant studies or guidelines on this topic.
Can macrolides be used to treat respiratory infections in children?
Share experiences or recommendations regarding the use of macrolide antibiotics in treating respiratory infections in children. Discuss any considerations or precautions that should be taken when using macrolides in pediatric patients.
What are the common side effects of macrolide antibiotics?
Explore and list the common side effects and adverse reactions associated with macrolide antibiotics. Share personal experiences or precautions to manage these side effects effectively.
Are macrolides a suitable choice for patients with penicillin allergies?
Discuss the suitability of prescribing macrolide antibiotics to patients allergic to penicillin. Share any guidelines or precautions when considering macrolides as an alternative in penicillin-allergic individuals.
Do macrolides interact with common medications?
Explore potential drug interactions between macrolide antibiotics and commonly used medications. Share any precautions or recommendations for patients who are taking macrolides along with other drugs.
Are macrolides effective in treating atypical pneumonia?
Discuss the efficacy of macrolide antibiotics in treating atypical pneumonia. Share any clinical experiences, studies, or guidelines supporting the use of macrolides for this specific type of respiratory infection.
What are the key differences between macrolides and other classes of antibiotics?
Compare and contrast macrolide antibiotics with other classes of antibiotics in terms of mechanism of action, spectrum of activity, common uses, and potential side effects. Share any unique characteristics that set macrolides apart from other antibiotic categories.
Are there any dietary restrictions when taking macrolide antibiotics?
Discuss if there are any specific dietary restrictions or considerations that patients should be aware of when taking macrolide antibiotics. Share any information on potential interactions between certain foods and macrolides.
How do macrolides compare to fluoroquinolones in treating respiratory infections?
Compare and contrast the efficacy and safety of macrolide antibiotics versus fluoroquinolones in the treatment of respiratory infections. Discuss any factors that influence the choice between these two classes of antibiotics for respiratory tract infections.