Customizing Antiviral Combination Therapies: A Targeted Approach
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-27
As the world grapples with an ever-evolving landscape of viral threats, the need for effective and tailored antiviral treatments has become increasingly pressing. Viruses, with their remarkable ability to mutate and adapt, often require a nuanced and strategic approach to combat their spread and severity. In this article, we will delve into the specific guidelines and considerations involved in crafting antiviral combination therapies that are tailored to the unique characteristics of different viral types.
At the heart of this discussion lies the fundamental understanding that a one-size-fits-all approach to antiviral therapy is seldom effective. Each virus possesses its own unique genetic makeup, resistance patterns, and mechanisms of infection, necessitating a customized response. By carefully analyzing the specific traits of a given virus, healthcare professionals can develop combination therapies that maximize the chances of successful treatment.
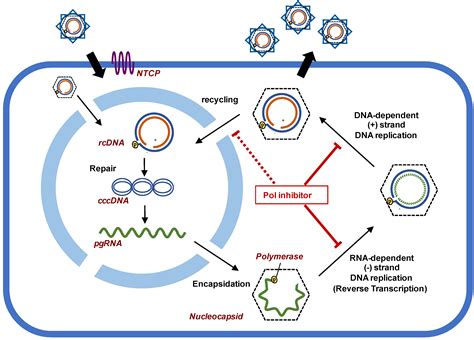
One of the primary considerations in tailoring antiviral combination therapies is the viral resistance profile. Viruses, much like bacteria, can develop resistance to individual antiviral agents over time, rendering certain drugs less effective. By combining multiple antiviral medications with different mechanisms of action, healthcare providers can create a synergistic effect that helps overcome these resistance barriers. This approach, known as combination therapy, not only enhances the potency of the treatment but also reduces the likelihood of the virus developing widespread resistance.
Another crucial factor in customizing antiviral therapies is the viral genotype or strain. Different viral strains may respond differently to various antiviral agents, and a treatment regimen that works well for one strain may be less effective against another. By conducting genetic analysis of the virus and assessing its susceptibility to different antiviral drugs, healthcare providers can select the most appropriate combination of medications to target the specific strain affecting the patient.
In addition to viral resistance and genotype, the route of transmission and the stage of infection also play a significant role in determining the optimal antiviral combination therapy. For instance, certain viruses may be more effectively targeted during the early stages of infection, while others may require a different approach to address the later stages of the disease. By understanding these nuances, healthcare professionals can tailor the treatment plan to the specific needs of the patient and the stage of the viral infection.
Furthermore, the patient's individual characteristics, such as their age, underlying health conditions, and drug metabolism, must be taken into account when selecting the appropriate antiviral combination. Certain medications may interact with other drugs the patient is taking or may not be well-tolerated by individuals with specific comorbidities. By considering these patient-specific factors, healthcare providers can minimize the risk of adverse effects and optimize the efficacy of the antiviral therapy.
In summary, the guidelines for tailoring antiviral combination therapies to different types of viruses are centered around a comprehensive understanding of the virus, its resistance patterns, genotype, transmission routes, and the patient's individual characteristics. By adopting a targeted and personalized approach to antiviral treatment, healthcare professionals can significantly improve patient outcomes and contribute to the ongoing battle against the ever-evolving viral landscape. As research and clinical experience continue to advance, we can expect to see even more refined and effective strategies for customizing antiviral combination therapies in the years to come.
What other factors do you believe should be considered when developing tailored antiviral combination therapies? Share your insights in the comments below.