Combating Skin Infections: Antibiotics vs. Antivirals
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Apr-12
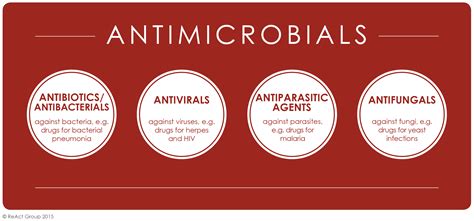
The skin is our body's first line of defense against the myriad of microbes that surround us daily. However, when this protective barrier is breached, various pathogens can infiltrate and cause troublesome skin infections. In such cases, healthcare providers often turn to two distinct classes of medications: antibiotics and antivirals. While both aim to alleviate skin infections, their mechanisms of action and specific targets differ significantly.
Antibiotics, the well-known workhorse in the fight against bacterial infections, work by either killing the offending bacteria or inhibiting their growth and replication. These medications target key cellular processes essential for bacterial survival, such as cell wall synthesis, protein production, or DNA replication. For example, penicillin interferes with the construction of the bacterial cell wall, causing the cells to rupture and die. In contrast, tetracyclines block the production of essential bacterial proteins, rendering the pathogens unable to thrive. By disrupting the fundamental biological functions of bacteria, antibiotics effectively eliminate the underlying cause of many skin infections, such as impetigo, cellulitis, and folliculitis.
On the other hand, antivirals are the go-to choice for managing viral skin infections. Unlike bacteria, viruses are not independent living organisms; instead, they rely on hijacking the host's cellular machinery to replicate and spread. Antivirals work by interfering with specific stages of the viral life cycle, preventing the pathogen from successfully infecting and reproducing within the host's cells. Some antivirals, such as acyclovir, block the viral enzyme responsible for DNA synthesis, while others, like oseltamivir, disrupt the release of new viral particles from infected cells. By targeting the unique vulnerabilities of viruses, antivirals can effectively curb the progression of conditions like herpes simplex, varicella-zoster (shingles), and molluscum contagiosum.
It is important to note that the choice between antibiotics and antivirals for skin infections is not a one-size-fits-all decision. Healthcare providers must carefully evaluate the clinical presentation, laboratory findings, and underlying causes to determine the most appropriate treatment approach. In some cases, a combination of both antibiotic and antiviral therapy may be necessary to address complex or co-occurring skin infections.
Moreover, the rise of antimicrobial resistance has underscored the importance of prudent and judicious use of these medications. Inappropriate or excessive use of antibiotics can lead to the emergence of resistant strains, rendering these once-effective drugs less potent. Similarly, the development of antiviral resistance can compromise the efficacy of these therapies. Healthcare providers must exercise caution and follow evidence-based guidelines to ensure the optimal management of skin infections while minimizing the risk of resistance.
As the field of dermatology continues to evolve, the interplay between antibiotics, antivirals, and skin infections remains a critical area of research and clinical practice. Understanding the nuances of these two distinct classes of medications can empower healthcare providers to make informed decisions and deliver tailored, effective treatments for their patients with skin infections. By staying vigilant and adapting to the changing landscape of microbial pathogens, we can improve the overall management and outcomes of these common, yet potentially challenging, skin conditions.
User comments
More Topics to Explore
Can antibiotics cause skin rashes?
Explore the connection between antibiotics and skin rashes, their possible causes, and how to manage this common side effect.
What are the risks of prolonged antibiotic use for skin infections?
Delve into the potential risks associated with prolonged antibiotic use for skin infections, including antibiotic resistance, allergic reactions, and disruption of the gut microbiome.
Can antibiotics for skin infections lead to yeast infections?
Examine the relationship between antibiotics used for skin infections and the development of yeast infections, including symptoms, prevention, and treatment options.
How can you minimize the side effects of antibiotics for skin infections?
Share strategies to minimize the side effects of antibiotics for skin infections, such as taking probiotics, staying hydrated, and following the prescribed dosage and duration.
Are there any natural alternatives to antibiotics for skin infections?
Discuss natural alternatives to antibiotics for skin infections, such as tea tree oil, honey, and essential oils, and their effectiveness in combating bacterial skin issues.