Adapting Antiviral Doses for Renal Compromise: A Delicate Balancing Act
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-15
As healthcare providers, we are often tasked with the challenge of ensuring optimal therapeutic outcomes for our patients, particularly when dealing with complex medical conditions. One such scenario is the management of antiviral medications in individuals with renal impairment. The kidneys play a crucial role in the elimination of many antiviral drugs, and alterations in renal function can significantly impact drug pharmacokinetics, necessitating appropriate dose adjustments.
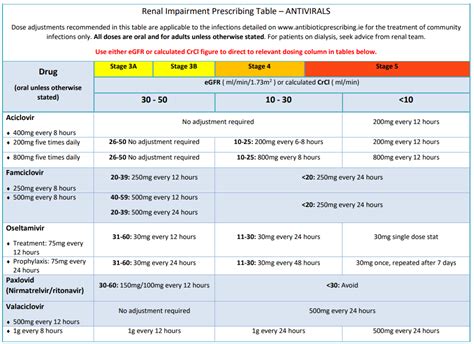
The dosage adjustments for antiviral medications in patients with renal impairment are guided by meticulous clinical research and well-established guidelines. These recommendations aim to strike a delicate balance between maintaining therapeutic efficacy and minimizing the risk of adverse events, such as drug toxicity.
For instance, in the case of nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs), which are commonly used for the treatment of HIV and hepatitis B, dose reductions are often necessary. The degree of dose adjustment is typically based on the patient's estimated glomerular filtration rate (eGFR), a measure of the kidney's filtration capacity. Similarly, protease inhibitors and non-nucleoside reverse transcriptase inhibitors may also require dose modifications in the setting of renal dysfunction.
In the realm of hepatitis C treatment, the direct-acting antivirals (DAAs) have revolutionized the landscape, offering highly effective and well-tolerated regimens. However, even these newer agents may necessitate dose adjustments in patients with renal impairment. For instance, the NS5A inhibitor ledipasvir has demonstrated the need for dose reduction in individuals with severe renal dysfunction.
It is worth noting that the specific dosage adjustments can vary across different antiviral medications and may also depend on the severity of renal impairment. Healthcare providers must carefully review the prescribing information and consult relevant clinical guidelines to ensure appropriate dose titration.
Beyond the pharmacological considerations, clinicians may also encounter unique challenges in the management of antiviral therapy in patients with renal impairment. These individuals often have complex medical histories, with the potential for multiple comorbidities and concomitant medications. Careful monitoring of drug interactions, adverse effects, and therapeutic response becomes paramount to optimize treatment outcomes.
In this context, the role of multidisciplinary collaboration cannot be overstated. Nephrologists, infectious disease specialists, and clinical pharmacists can work together to develop personalized treatment plans that address the unique needs of each patient, ensuring the safe and effective use of antiviral medications.
As we continue to navigate the evolving landscape of antiviral therapy, the importance of understanding the appropriate dose adjustments for renal impairment remains a critical component of providing high-quality, patient-centered care. By staying abreast of the latest clinical guidelines and fostering interdisciplinary cooperation, healthcare providers can strive to deliver the best possible outcomes for their patients.
What are your experiences or insights regarding the management of antiviral medications in patients with renal impairment? We welcome your thoughts and perspectives on this important clinical challenge.