Changing HIV Medications: A Delicate Transition
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Apr-06
The management of HIV (Human Immunodeficiency Virus) is a dynamic and ever-evolving field, requiring healthcare providers to carefully navigate the complexities of antiretroviral therapy (ART). One of the critical aspects of this journey is the process of switching antiviral medications, a decision that demands meticulous consideration to ensure the continued effectiveness of treatment and the well-being of the patient.
When it comes to transitioning between different antiviral medications, several key factors come into play. Firstly, the underlying reason for the medication change must be thoroughly evaluated. This may include the development of drug resistance, the occurrence of adverse side effects, or the need to simplify the treatment regimen. Understanding the specific clinical scenario is paramount, as it will guide the healthcare team in selecting the most appropriate alternative therapy.
One of the primary concerns when switching HIV medications is the potential for cross-resistance, where the patient's virus may have developed resistance to multiple drugs within the same class. This can significantly limit the available treatment options and increase the risk of treatment failure. Careful review of the patient's resistance profile, often through genotypic resistance testing, is essential to ensure that the new regimen is likely to be effective.
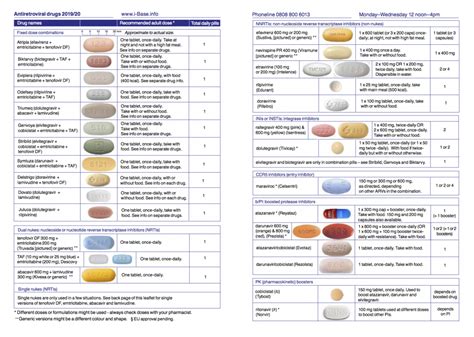
Another crucial aspect to consider is the potential drug interactions between the new antiviral medication and any other medications the patient may be taking, including prescription drugs, over-the-counter supplements, or even certain foods. These interactions can alter the pharmacokinetics of the medications, potentially leading to reduced efficacy or increased toxicity. Healthcare providers must meticulously review the patient's medication history and carefully select the new regimen to minimize the risk of harmful interactions.
The timing of the medication switch is also a critical factor. Ideally, the transition should occur when the patient's viral load is well-controlled, minimizing the risk of viral rebound or the development of additional resistance mutations. In some cases, a "bridging" strategy may be employed, where the patient is temporarily maintained on their current regimen while the new medications are introduced, allowing for a gradual and seamless transition.
Perhaps one of the most significant challenges during the transition process is the management of the patient's psychological well-being. Changing HIV medications can be a source of anxiety and uncertainty for many individuals, as they may fear the potential impact on their health and quality of life. Healthcare providers must prioritize clear communication, providing comprehensive education and emotional support to the patient throughout the process. This can help to alleviate concerns, foster trust, and ultimately improve the patient's adherence to the new regimen.
In conclusion, switching antiviral medications for HIV treatment is a complex and delicate process that requires the utmost care and consideration. By addressing the underlying reasons for the change, evaluating the risk of cross-resistance, managing potential drug interactions, and prioritizing the patient's psychological well-being, healthcare providers can help to ensure a successful and seamless transition, ultimately contributing to the long-term success of the patient's HIV management strategy. As the field of HIV care continues to evolve, staying informed and adaptable is crucial for healthcare professionals to provide the best possible care for their patients.
What factors do you consider most important when transitioning between different antiviral medications for HIV treatment? Share your thoughts and experiences in the comments below.