Herpes: Navigating the Complexities of Episodic and Suppressive Antiviral Therapy
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-27
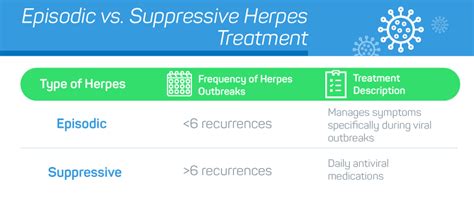
The management of herpes, a chronic viral infection, often requires a strategic approach to effectively control its symptoms and prevent future outbreaks. Two primary treatment options have emerged, each with its own unique characteristics and considerations – episodic and suppressive antiviral therapy. Understanding the differences between these approaches is crucial for healthcare providers and patients alike.
Episodic Antiviral Therapy for Herpes
Episodic antiviral therapy is designed to address the acute phase of a herpes outbreak, aiming to alleviate symptoms and expedite the healing process. This approach is typically recommended for individuals who experience infrequent or occasional herpes outbreaks. The patient is instructed to initiate the antiviral medication as soon as they recognize the initial signs of an impending outbreak, such as tingling, burning, or the appearance of blisters. Common antiviral medications used in episodic therapy include acyclovir, valacyclovir, and famciclovir, often prescribed for a duration of 5-10 days.
The benefits of episodic antiviral therapy lie in its ability to shorten the duration and severity of an active herpes outbreak. By intervening early, the medications can help reduce the intensity of symptoms, accelerate the healing of lesions, and potentially decrease the risk of viral transmission to partners. This approach is particularly useful for individuals who experience infrequent flare-ups and seek to manage their symptoms effectively during these episodes.
Suppressive Antiviral Therapy for Herpes
In contrast, suppressive antiviral therapy aims to prevent or reduce the frequency of herpes outbreaks over an extended period. This long-term treatment strategy is often recommended for individuals who experience recurrent or frequent herpes outbreaks, typically defined as four or more episodes per year. The same antiviral medications used in episodic therapy – acyclovir, valacyclovir, and famciclovir – are prescribed, but in lower, continuous doses.
The primary benefit of suppressive antiviral therapy is its ability to significantly reduce the number and severity of herpes outbreaks. By maintaining a constant level of the antiviral medication in the body, the virus is effectively suppressed, leading to a decrease in both the frequency and intensity of future flare-ups. This approach can also have a positive impact on an individual's quality of life, as it minimizes the disruption and discomfort associated with recurring herpes episodes.
Moreover, suppressive antiviral therapy has been shown to reduce the risk of viral transmission to sexual partners, making it a valuable tool in preventing the spread of herpes within relationships. The continuous treatment regimen requires regular medication adherence, often for an indefinite period, to maintain its efficacy.
Choosing the Appropriate Approach
The decision to opt for episodic or suppressive antiviral therapy for herpes should be made in collaboration with a healthcare provider, considering the individual's unique circumstances, the frequency and severity of their outbreaks, and their personal preferences. Factors such as the patient's overall health, the impact of herpes on their quality of life, and the potential risks and benefits of each approach should be carefully evaluated.
In some cases, individuals may transition from episodic to suppressive therapy if their outbreak patterns become more frequent or severe over time. Conversely, those who experience infrequent outbreaks may find episodic therapy more suitable and cost-effective.
Ultimately, the goal of both episodic and suppressive antiviral therapy is to empower individuals with herpes to manage their condition effectively, minimize the burden of the disease, and maintain a healthy, fulfilling life. By understanding the nuances of these treatment options, patients and healthcare providers can collaborate to devise the most appropriate and personalized approach to addressing the challenges of herpes.