What are the key considerations when prescribing antibiotics to children?
When it comes to prescribing antibiotics for children in primary care, what are the key factors healthcare providers should consider? Share best practices and tips for safe antibiotic use in paediatric patients.
Antibiotic Considerations in Pediatric Patients: A Delicate Balance
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-21
As healthcare providers, we are often tasked with the responsibility of prescribing antibiotics to our youngest patients - the children under our care. This decision carries significant weight, as the use of these powerful medications in the pediatric population requires a nuanced approach. When it comes to prescribing antibiotics for children in primary care, there are several key factors that healthcare providers must carefully consider.
The first and foremost consideration is the appropriate diagnosis. Children are susceptible to a wide range of bacterial infections, from streptococcal pharyngitis to urinary tract infections. However, it is crucial to distinguish these bacterial infections from viral illnesses, which do not typically require antibiotic treatment. Relying on clinical presentation, laboratory tests, and evidence-based guidelines can help ensure that antibiotics are prescribed only when truly necessary.
Once the diagnosis is established, healthcare providers must then evaluate the appropriate antibiotic selection. Factors such as the child's age, weight, and underlying medical conditions, as well as the specific pathogen and its antibiotic susceptibility, should all be taken into account. Selecting the right antibiotic can help optimize treatment efficacy while minimizing the risk of antibiotic resistance and adverse events.
Another critical consideration is the dosage and duration of treatment. Pediatric patients often require different dosing regimens compared to adults, as their pharmacokinetics and pharmacodynamics can vary significantly. Healthcare providers must carefully calculate the appropriate dose based on the child's weight and adjust it as necessary throughout the course of treatment. Additionally, the duration of antibiotic therapy should be the shortest effective period, as prolonged use can contribute to the development of antibiotic-resistant bacteria.
Addressing the potential for adverse effects is another key factor in prescribing antibiotics for children. Certain antibiotics, such as fluoroquinolones, have been associated with an increased risk of musculoskeletal complications in young patients. Healthcare providers must carefully weigh the benefits and risks of each antibiotic and monitor for any adverse events during the course of treatment.
Finally, the importance of patient education and shared decision-making cannot be overstated. Engaging parents or caregivers in the decision-making process and providing clear instructions on antibiotic use, potential side effects, and the importance of completing the full course of therapy can help foster better adherence and improve overall outcomes.
In summary, prescribing antibiotics to children in primary care requires a delicate balance of clinical expertise, evidence-based practices, and patient-centered care. By carefully considering the appropriate diagnosis, antibiotic selection, dosage and duration, potential adverse effects, and engaging in shared decision-making with families, healthcare providers can help ensure the safe and effective use of these powerful medications in the pediatric population. Maintaining this balanced approach is crucial in the ongoing effort to combat the growing threat of antibiotic resistance and promote the best possible outcomes for our young patients.
User comments
More Topics to Explore
Can antibiotics be safely prescribed over the phone?
With the rise of telemedicine, is it safe and appropriate to prescribe antibiotics over the phone without physically examining the patient? Share your thoughts and experiences.
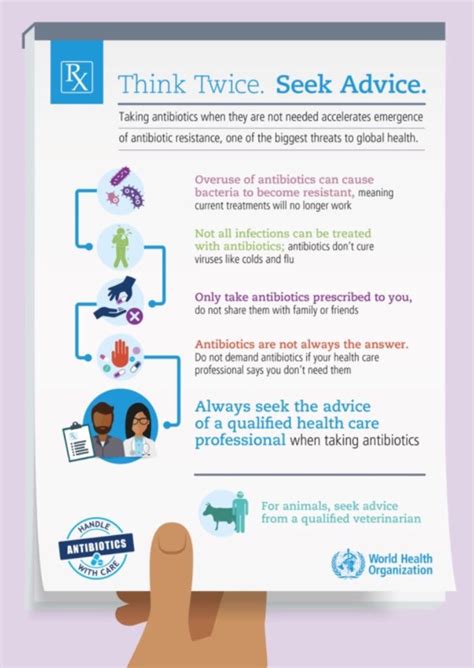
Are antibiotics being overprescribed in primary care?
Are healthcare providers overprescribing antibiotics in primary care settings? Join the discussion on the impact of overprescription and how we can promote better antibiotic stewardship.
How can primary care providers effectively communicate antibiotic resistance to patients?
Antibiotic resistance is a growing concern. How can primary care providers effectively educate patients about this issue while ensuring appropriate antibiotic use? Share your strategies and experiences.
What role do pharmacists play in optimizing antibiotic use in primary care?
Pharmacists are key players in promoting appropriate antibiotic use. How can pharmacists support primary care providers in optimizing antibiotic prescribing and educating patients? Share insights and collaboration ideas.
Are there effective alternatives to antibiotics for common primary care infections?
In cases where antibiotics may not be necessary, what are some effective alternative treatments for common infections seen in primary care? Share evidence-based alternatives and when they may be appropriate.
How should primary care providers approach antibiotic prescribing for elderly patients?
Prescribing antibiotics for elderly patients in primary care requires special considerations. What are the key factors healthcare providers should keep in mind when treating infections in the elderly population?
What are the current guidelines for antibiotic use in primary care settings?
Stay up-to-date on the latest guidelines for antibiotic use in primary care. Discuss the recommended practices, common misconceptions, and challenges in adhering to guidelines when prescribing antibiotics.
What impact does antibiotic resistance have on primary care practice?
Antibiotic resistance is a global health threat. How does antibiotic resistance impact primary care practice, and what strategies can healthcare providers implement to combat this issue?