What impact does antibiotic resistance have on primary care practice?
Antibiotic resistance is a global health threat. How does antibiotic resistance impact primary care practice, and what strategies can healthcare providers implement to combat this issue?
Tackling the Antibiotic Resistance Challenge in Primary Care
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Apr-12
Antibiotic resistance is a growing global health concern that healthcare providers cannot afford to ignore. As primary care practitioners on the frontlines of patient care, understanding the impact of this threat and implementing effective strategies is crucial for delivering quality, sustainable healthcare.
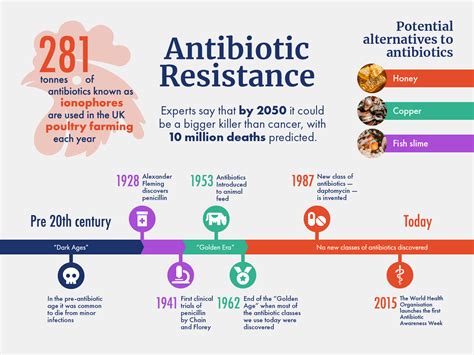
At the heart of the issue lies the overuse and misuse of antibiotics, which has contributed to the emergence of drug-resistant pathogens. These superbugs can no longer be reliably treated with once-effective antimicrobial drugs, posing significant risks to patient outcomes. In the primary care setting, this translates to more complex, prolonged, and potentially untreatable infections.
One key impact is the increased burden on primary care practices. Resistant infections often require more extensive diagnostic testing, longer treatment durations, and closer monitoring - all of which strain limited resources and can lead to patient backlog. Additionally, the lack of reliable antibiotic options may necessitate referrals to specialists, adding to the workload and costs for both patients and providers.
Furthermore, antibiotic resistance can undermine the ability of primary care clinicians to effectively manage common conditions. Routine procedures like joint replacements, cancer treatments, and even childbirth carry heightened risks of healthcare-associated infections that may be difficult to treat. This can significantly impact patient trust and satisfaction, as well as healthcare delivery as a whole.
To combat this challenge, primary care providers must adopt a multifaceted approach. Firstly, judicious antibiotic stewardship is crucial - carefully evaluating the need for antimicrobial therapy, prescribing the narrowest-spectrum agent, and ensuring appropriate duration of treatment. Educating patients on the importance of completing prescribed courses and avoiding unnecessary requests for antibiotics is also vital.
Implementing robust infection prevention and control measures, such as hand hygiene, environmental cleaning, and vaccination programs, can help minimize the spread of resistant pathogens within the primary care setting. Collaboration with public health authorities to monitor resistance trends and coordinate response efforts is another key strategy.
Finally, primary care providers must stay informed about emerging diagnostic tools and treatment options for resistant infections. Leveraging rapid molecular tests to identify pathogens and guide antibiotic selection can improve clinical decision-making and patient outcomes. Exploring alternative therapies, such as phage therapy or novel antimicrobial compounds, may also prove valuable in the fight against superbugs.
By embracing these strategies, primary care practitioners can play a vital role in curbing the tide of antibiotic resistance and ensuring the continued effectiveness of these essential medications. As we navigate this complex challenge, one thing is clear: the future of primary care depends on our ability to adapt and innovate in the face of this global health threat.
What steps is your primary care practice taking to address the issue of antibiotic resistance? We'd be curious to hear your insights and experiences.
User comments
More Topics to Explore
Can antibiotics be safely prescribed over the phone?
With the rise of telemedicine, is it safe and appropriate to prescribe antibiotics over the phone without physically examining the patient? Share your thoughts and experiences.
Are antibiotics being overprescribed in primary care?
Are healthcare providers overprescribing antibiotics in primary care settings? Join the discussion on the impact of overprescription and how we can promote better antibiotic stewardship.
What are the key considerations when prescribing antibiotics to children?
When it comes to prescribing antibiotics for children in primary care, what are the key factors healthcare providers should consider? Share best practices and tips for safe antibiotic use in paediatric patients.
How can primary care providers effectively communicate antibiotic resistance to patients?
Antibiotic resistance is a growing concern. How can primary care providers effectively educate patients about this issue while ensuring appropriate antibiotic use? Share your strategies and experiences.
What role do pharmacists play in optimizing antibiotic use in primary care?
Pharmacists are key players in promoting appropriate antibiotic use. How can pharmacists support primary care providers in optimizing antibiotic prescribing and educating patients? Share insights and collaboration ideas.
Are there effective alternatives to antibiotics for common primary care infections?
In cases where antibiotics may not be necessary, what are some effective alternative treatments for common infections seen in primary care? Share evidence-based alternatives and when they may be appropriate.
How should primary care providers approach antibiotic prescribing for elderly patients?
Prescribing antibiotics for elderly patients in primary care requires special considerations. What are the key factors healthcare providers should keep in mind when treating infections in the elderly population?
What are the current guidelines for antibiotic use in primary care settings?
Stay up-to-date on the latest guidelines for antibiotic use in primary care. Discuss the recommended practices, common misconceptions, and challenges in adhering to guidelines when prescribing antibiotics.