The Diverging Paths of Antiviral and Antibacterial Resistance
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Apr-09
Resistance is a concerning issue that has significant implications for public health, impacting our ability to effectively treat infections caused by both viruses and bacteria. While antiviral resistance and antibacterial resistance may seem similar on the surface, there are some profound distinctions between the two that are crucial to understand.
At the most fundamental level, the mechanisms by which viruses and bacteria develop resistance differ considerably. Viruses, being obligate intracellular parasites, leverage the host cell's machinery to replicate and spread. Antiviral resistance often arises through genetic mutations that allow the virus to evade the effects of antiviral drugs, altering key viral proteins or enzymes. This can reduce the efficacy of antiviral medications, rendering them less effective at stopping viral replication and transmission.
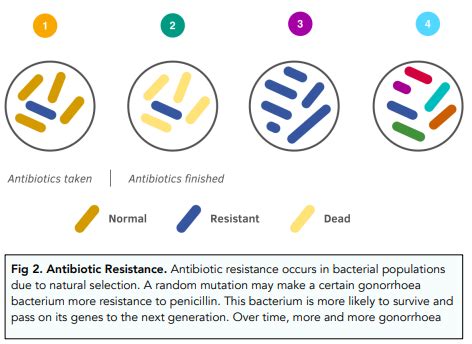
In contrast, bacteria are free-living microorganisms that possess their own metabolic processes and genetic material. Antibacterial resistance typically emerges through the acquisition of genetic elements, such as plasmids or transposons, that confer resistance mechanisms. These can include the production of enzymes that inactivate antibiotics, alterations to antibiotic target sites, or the enhancement of efflux pumps that expel the antibiotics from the bacterial cell.
The rate at which resistance can develop also varies between viruses and bacteria. Viruses, with their rapid replication cycles and high mutation rates, can evolve resistance more quickly in response to selective pressures imposed by antiviral drugs. Bacteria, while possessing a slower replication pace, can still readily acquire resistance genes through horizontal gene transfer, allowing for the rapid spread of resistance within and between bacterial populations.
Another key difference lies in the breadth of resistance. Antibacterial resistance often manifests as multidrug resistance, where bacteria become resistant to multiple classes of antibiotics. This can severely limit treatment options and lead to the emergence of superbugs - bacteria that are resistant to almost all available antibiotics. In contrast, antiviral resistance tends to be more specific, with viruses becoming resistant to particular antiviral agents rather than entire drug classes.
The consequences of antiviral and antibacterial resistance also differ in their clinical implications. Viral infections, while potentially severe, are generally self-limiting and can often be managed through supportive care. Bacterial infections, on the other hand, can be life-threatening if left untreated, and the rise of multidrug-resistant bacteria poses a grave threat to public health.
In conclusion, while both antiviral and antibacterial resistance pose significant challenges, the underlying mechanisms, rates of development, and clinical impacts vary considerably. Understanding these distinctions is crucial for the development of effective strategies to combat the growing threat of antimicrobial resistance.
So, what do you think - are there any other key differences between antiviral and antibacterial resistance that are worth exploring? Let us know your thoughts in the comments below!