Maintaining Strong Bones: Navigating the Impacts of Long-Term Antibiotic and Antiviral Use in Older Adults
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Apr-09
As we age, preserving our bone health becomes increasingly vital. However, for many older adults, long-term use of antibiotics and antivirals can pose a unique challenge to this goal. The potential effects of these medications on bone density and fracture risk have garnered significant attention from the medical community, prompting a deeper examination of this complex issue.
Antibiotics, often prescribed to treat a wide range of infectious diseases, have been linked to adverse effects on bone health. Prolonged use of certain antibiotic classes, such as fluoroquinolones and tetracyclines, has been associated with an increased risk of osteoporosis and bone fractures. The proposed mechanisms behind this relationship involve disruptions in the balance of bone formation and resorption, as well as alterations in the gut microbiome, which play a crucial role in calcium and vitamin D absorption.
Similarly, antiviral medications, used to manage conditions like HIV/AIDS, hepatitis, and more recently, COVID-19, have also been implicated in bone health concerns. Some antivirals have been shown to interfere with the activity of osteoblasts (cells responsible for bone formation) and osteoclasts (cells that break down bone), leading to a potential imbalance in bone remodeling. Additionally, the underlying medical conditions that require antiviral therapy, such as chronic viral infections, may themselves contribute to an increased risk of osteoporosis.
The impact of these medications on bone health can be particularly pronounced in older adults, who already face a heightened risk of osteoporosis and fragility fractures due to age-related changes in bone metabolism. Compounding this issue, many older individuals also have comorbidities, such as diabetes, kidney disease, or malnutrition, which can further exacerbate the negative effects of long-term antibiotic and antiviral use on bone health.
1. Bone Density Monitoring: Regular dual-energy X-ray absorptiometry (DEXA) scans to assess bone mineral density and monitor for early signs of osteoporosis.
2. Nutritional Interventions: Ensuring adequate intake of calcium, vitamin D, protein, and other bone-supportive nutrients through dietary modifications or supplementation.
3. Physical Activity Recommendations: Encouraging weight-bearing exercises and activities that promote muscle strength and balance, which can help reduce the risk of falls and fractures.
4. Medication Management: Carefully evaluating the necessity and duration of antibiotic and antiviral therapies, and considering alternative options that may have less impact on bone health.
5. Collaboration with Specialists: Referring patients to endocrinologists, rheumatologists, or geriatric specialists for comprehensive bone health assessments and targeted interventions.
By implementing these strategies and fostering a collaborative approach between healthcare providers and older adults, we can strive to mitigate the potential adverse effects of long-term antibiotic and antiviral use on bone health, and empower individuals to maintain strong, resilient bones well into their golden years.
User comments
More Topics to Explore
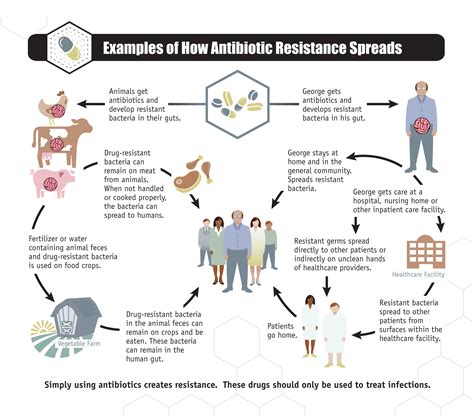
What are the risks of antibiotic resistance in older adults?
Explore the dangers of antibiotic resistance in the elderly population and ways to mitigate this growing health concern.