What impact do Antibiotic Stewardship Programs have on reducing healthcare costs?
Analyze the economic benefits of Antibiotic Stewardship Programs in terms of cost savings for healthcare institutions and the broader impact on healthcare expenditures.
Antibiotic Stewardship Programs: Unlocking Cost Savings in Healthcare
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Apr-09
The rise of antibiotic-resistant bacteria has become a global health crisis, posing a significant threat to patient safety and healthcare costs. In response, healthcare institutions have implemented Antibiotic Stewardship Programs (ASPs) to promote the judicious use of antibiotics, but what impact do these programs have on reducing healthcare expenditures?
Antibiotics are undoubtedly essential in modern medicine, treating a wide range of infections and saving countless lives. However, their overuse and misuse have contributed to the alarming spread of antibiotic-resistant pathogens, which can be difficult and expensive to treat. This has led to a growing recognition that a more thoughtful approach to antibiotic prescribing is needed.
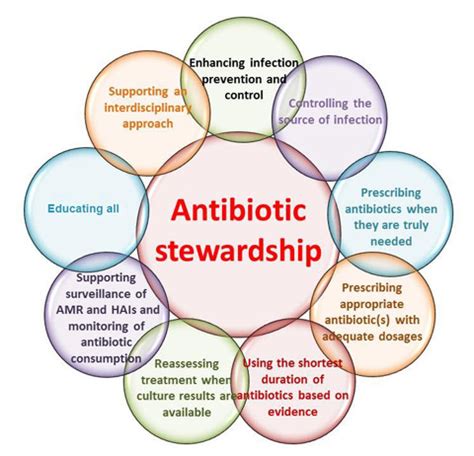
Enter Antibiotic Stewardship Programs. These initiatives, often led by a multidisciplinary team of healthcare professionals, aim to optimize the use of antibiotics by developing evidence-based guidelines, providing education and feedback to prescribers, and monitoring antibiotic usage patterns. The ultimate goal is to improve patient outcomes, reduce the development of antibiotic resistance, and, crucially, lower healthcare costs.
The economic benefits of ASPs are well-documented. Several studies have demonstrated that these programs can generate significant cost savings for healthcare institutions. By reducing the unnecessary or inappropriate use of antibiotics, ASPs can lead to decreased expenditures on antibiotic medications, as well as the associated costs of treating antibiotic-resistant infections and their complications.
One meta-analysis, published in the *Clinical Infectious Diseases* journal, analyzed the impact of ASPs across 32 studies and found an average cost savings of $200,000 per hospital per year. The savings came from various sources, including reduced antibiotic expenditures, shorter hospital stays, and lower rates of Clostridioides difficile (C. diff) infection, a serious and costly complication of antibiotic use.
Moreover, the benefits of ASPs extend beyond the individual healthcare institution. Reducing the development of antibiotic resistance can have a broader impact on healthcare expenditures. When antibiotic-resistant infections are less prevalent, the need for more expensive, last-resort antibiotics and the associated costs of managing these infections can be significantly decreased.
A study published in the *Journal of the American Medical Association* estimated that the annual cost of antibiotic-resistant infections in the United States is between $21 billion and $34 billion. By curbing the spread of antibiotic resistance, ASPs can contribute to substantial savings for the entire healthcare system.
Despite the compelling evidence for the economic benefits of Antibiotic Stewardship Programs, their implementation is not without challenges. Securing the necessary resources, overcoming potential resistance from prescribers, and demonstrating the long-term financial impact can all be hurdles that healthcare institutions must navigate.
Nevertheless, the potential for cost savings is undeniable. As healthcare systems continue to grapple with the rising costs of healthcare, Antibiotic Stewardship Programs offer a promising solution that can improve patient outcomes, curb the threat of antibiotic resistance, and ultimately, reduce the financial burden on the healthcare system. The question remains: How can more healthcare institutions leverage the power of these programs to achieve sustainable cost savings?
User comments
More Topics to Explore
How can Antibiotic Stewardship Programs help combat resistant infections?
Discuss the role of Antibiotic Stewardship Programs in addressing the challenge of resistant infections and share strategies for their effective implementation.
What are the key components of successful Antibiotic Stewardship Programs?
Explore the essential elements that make Antibiotic Stewardship Programs effective in managing antibiotic use and combating resistant infections.
How can healthcare professionals promote Antibiotic Stewardship in their practice?
Share tips and best practices for healthcare professionals to advocate for and implement Antibiotic Stewardship Programs in their clinical settings.
What role do patients play in supporting Antibiotic Stewardship efforts?
Discuss the importance of patient engagement in Antibiotic Stewardship Programs and ways patients can contribute to combating resistant infections.
How do Antibiotic Stewardship Programs contribute to reducing antibiotic resistance?
Delve into the connection between Antibiotic Stewardship Programs and the decline of antibiotic resistance, and share success stories of their impact.
What challenges do healthcare facilities face when implementing Antibiotic Stewardship Programs?
Examine the obstacles healthcare institutions encounter when establishing Antibiotic Stewardship Programs and discuss solutions to overcome these challenges.
Are there specific guidelines for designing Antibiotic Stewardship Programs in different healthcare settings?
Explore the tailored approaches for developing Antibiotic Stewardship Programs in various healthcare environments and the guidelines that support their implementation.
How can technology support Antibiotic Stewardship initiatives?
Dive into the role of technology and innovation in enhancing Antibiotic Stewardship efforts and discuss the latest advancements in digital tools for antibiotic management.
Can community outreach programs improve public awareness of Antibiotic Stewardship?
Examine the role of community outreach programs in raising awareness about Antibiotic Stewardship and discuss effective strategies for engaging the public in responsible antibiotic use.