What role do patients play in supporting Antibiotic Stewardship efforts?
Discuss the importance of patient engagement in Antibiotic Stewardship Programs and ways patients can contribute to combating resistant infections.
Patients as Partners in Antibiotic Stewardship
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-24
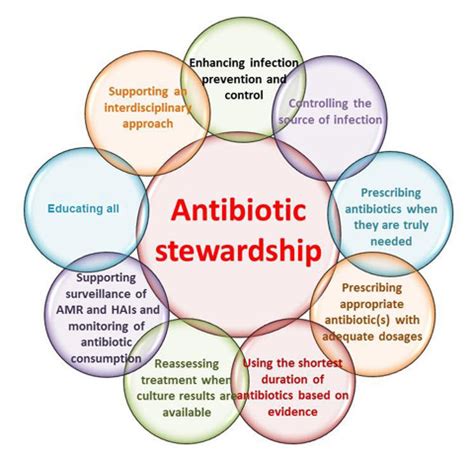
The steady rise of antibiotic-resistant infections poses a serious threat to global health, with the potential to significantly undermine our ability to treat common bacterial illnesses. In response, healthcare facilities around the world have implemented Antibiotic Stewardship Programs (ASPs) - proactive initiatives aimed at optimizing antibiotic use and curbing the spread of resistant pathogens. While these programs primarily involve clinicians, pharmacists, and infection prevention specialists, a crucial element often overlooked is the role of patients themselves.
Patients, as the ultimate consumers of antibiotics, wield significant influence over antibiotic usage patterns. Their knowledge, attitudes, and behaviors can either support or undermine the goals of Antibiotic Stewardship. By actively engaging patients in these stewardship efforts, healthcare providers have an opportunity to harness patient power and establish a collaborative partnership in the fight against antimicrobial resistance.
One of the most important ways patients can contribute is by developing a better understanding of antibiotic resistance and the appropriate use of these medications. Many patients harbor misconceptions about antibiotics, believing they are effective against viral infections or that they should complete a course of antibiotics even if they feel better. Educational initiatives that empower patients to make more informed decisions about antibiotic use can go a long way in reducing unnecessary prescriptions and curbing the development of resistance.
Patients can also play a vital role in ensuring proper antibiotic adherence - taking the medication as directed and completing the full course of treatment. Incomplete or irregular antibiotic use is a significant driver of resistance, as it allows bacteria to adapt and develop survival mechanisms. By encouraging patients to follow their antibiotic regimen, healthcare providers can minimize the risk of treatment failure and the emergence of resistant strains.
Another key area where patient engagement is crucial is infection prevention and control. Patients can help prevent the spread of resistant infections by adhering to good hand hygiene practices, following isolation protocols when necessary, and reporting any suspected healthcare-associated infections. Their active participation in these preventive measures can complement the efforts of clinical staff and enhance the overall efficacy of Antibiotic Stewardship Programs.
Lastly, patients can contribute to ASPs by serving as advocates and ambassadors, raising awareness about antibiotic resistance and the importance of responsible antibiotic use within their communities. By sharing their personal experiences and perspectives, patients can help shift social norms and foster a broader culture of antibiotic stewardship.
As healthcare systems continue to grapple with the challenge of antimicrobial resistance, the inclusion of patients as active partners in Antibiotic Stewardship Programs will be increasingly crucial. By empowering patients to make informed choices, adhere to treatment, and engage in preventive behaviors, we can harness the collective power of the patient population to combat this global threat and safeguard the effectiveness of our most valuable medical tools. What other ways can patients contribute to Antibiotic Stewardship efforts in your community?
User comments
More Topics to Explore
How can Antibiotic Stewardship Programs help combat resistant infections?
Discuss the role of Antibiotic Stewardship Programs in addressing the challenge of resistant infections and share strategies for their effective implementation.
What are the key components of successful Antibiotic Stewardship Programs?
Explore the essential elements that make Antibiotic Stewardship Programs effective in managing antibiotic use and combating resistant infections.
How can healthcare professionals promote Antibiotic Stewardship in their practice?
Share tips and best practices for healthcare professionals to advocate for and implement Antibiotic Stewardship Programs in their clinical settings.
How do Antibiotic Stewardship Programs contribute to reducing antibiotic resistance?
Delve into the connection between Antibiotic Stewardship Programs and the decline of antibiotic resistance, and share success stories of their impact.
What challenges do healthcare facilities face when implementing Antibiotic Stewardship Programs?
Examine the obstacles healthcare institutions encounter when establishing Antibiotic Stewardship Programs and discuss solutions to overcome these challenges.
Are there specific guidelines for designing Antibiotic Stewardship Programs in different healthcare settings?
Explore the tailored approaches for developing Antibiotic Stewardship Programs in various healthcare environments and the guidelines that support their implementation.
How can technology support Antibiotic Stewardship initiatives?
Dive into the role of technology and innovation in enhancing Antibiotic Stewardship efforts and discuss the latest advancements in digital tools for antibiotic management.
What impact do Antibiotic Stewardship Programs have on reducing healthcare costs?
Analyze the economic benefits of Antibiotic Stewardship Programs in terms of cost savings for healthcare institutions and the broader impact on healthcare expenditures.
Can community outreach programs improve public awareness of Antibiotic Stewardship?
Examine the role of community outreach programs in raising awareness about Antibiotic Stewardship and discuss effective strategies for engaging the public in responsible antibiotic use.