What impact does antibiotic resistance have on the efficacy of combination therapy approaches?
Discuss the correlation between antibiotic resistance and the effectiveness of combination therapy in combating resistant infections. Share your thoughts on how the rise of antibiotic resistance influences the success of combination treatment strategies.
Antibiotic Resistance and Combination Therapy: A Concerning Intersection
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-30
The rise of antibiotic resistance has posed a significant challenge to the medical community, rendering once-reliable treatments less effective in combating infectious diseases. As the prevalence of drug-resistant pathogens continues to grow, healthcare professionals have turned to combination therapy approaches in hopes of overcoming this pressing issue. However, the relationship between antibiotic resistance and the efficacy of combination therapy is a complex and concerning one.
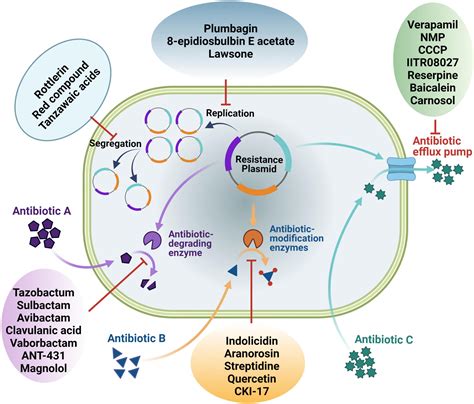
Antibiotic resistance occurs when bacteria, viruses, or other microorganisms develop the ability to withstand the effects of antimicrobial drugs. This can happen through various mechanisms, such as the production of enzymes that inactivate the drugs, the modification of drug targets, or the development of efflux pumps that expel the drugs from the cells. As antibiotic resistance spreads, previously effective treatments become less reliable, leaving healthcare providers with fewer options to combat serious infections.
In this context, combination therapy has emerged as a potential solution. The idea behind combination therapy is to use a combination of two or more antimicrobial agents that target different mechanisms or pathways in the pathogen, making it more difficult for the microorganism to develop resistance to all the drugs simultaneously. This approach has shown promising results in certain scenarios, as the synergistic effects of the combined therapies can enhance the overall antimicrobial activity and potentially overcome antibiotic resistance.
However, the effectiveness of combination therapy is not without its challenges when it comes to antibiotic resistance. As pathogens continue to evolve and adapt, they may develop resistance to multiple antimicrobial agents, rendering combination therapy less effective. Additionally, the complex pharmacokinetics and pharmacodynamics of combination therapies can make it challenging to optimize the dosing and timing of the various drugs, which may further contribute to the development of resistance.
Moreover, the use of combination therapy can also have unintended consequences, such as the selection of even more resistant strains or the emergence of new, more virulent pathogens. This is particularly concerning in healthcare settings, where the high use of antimicrobial agents and the close proximity of patients can create an environment that facilitates the spread of resistant infections.
In conclusion, the relationship between antibiotic resistance and the efficacy of combination therapy is a complex and concerning issue. While combination therapy holds promise as a means of overcoming resistant infections, the continued evolution of pathogens and the complex dynamics of antimicrobial use pose significant challenges. Addressing this problem will require a multifaceted approach, including the development of new antimicrobial agents, the optimization of existing combination therapies, and the implementation of robust stewardship programs to ensure the judicious use of antibiotics. Only through a collaborative effort can we hope to effectively tackle the threat of antibiotic resistance and ensure the continued effectiveness of our treatment options.
How can healthcare providers and researchers work together to address the challenges posed by the intersection of antibiotic resistance and combination therapy approaches? What innovative strategies might be explored to enhance the long-term success of combination therapy in the face of evolving resistant pathogens?
User comments
More Topics to Explore
How effective are combination therapy approaches in treating resistant infections?
Discuss the efficacy of combination therapy in combating resistant infections and share your experiences and opinions on its effectiveness.
What are the potential advantages of using combination therapy over single-agent therapy for resistant infections?
Delve into the benefits of utilizing combination therapy over single-agent therapy for combating resistant infections. Share your knowledge and thoughts on the advantages of this treatment approach.
Are there any challenges or risks associated with using combination therapy for resistant infections?
Explore the potential challenges and risks that come with employing combination therapy in the treatment of resistant infections. Share cautionary tales or experiences to enlighten others on the drawbacks of this approach.
In what scenarios would combination therapy be more beneficial than monotherapy for resistant infections?
Share your expertise on situations where implementing combination therapy proves to be more advantageous than monotherapy in treating resistant infections. Discuss specific cases or examples to illustrate the superiority of this treatment approach.
How can healthcare professionals optimize combination therapy approaches to combat emerging resistant infections effectively?
Exchange ideas and strategies on how healthcare professionals can enhance the utilization of combination therapy to tackle emerging resistant infections. Share best practices and insights to optimize treatment outcomes.
What role do antimicrobial stewardship programs play in promoting the appropriate use of combination therapy for resistant infections?
Delve into the significance of antimicrobial stewardship programs in advocating for the judicious application of combination therapy for resistant infections. Share insights on how these programs influence the decision-making process in treatment selection.
What evidence-based practices support the use of combination therapy approaches in combating resistant infections?
Explore the foundational evidence and research backing the efficacy of combination therapy in addressing resistant infections. Share empirical findings and studies that support the adoption of combination approaches in clinical practice.