Why are some Viruses more Prone to Developing Resistance to Antiviral Medications?
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-15
Viruses are fascinating yet incredibly complex microscopic entities that have the remarkable ability to replicate and evolve within their host organisms. While modern medicine has made significant strides in developing antiviral medications to combat various viral infections, the incessant evolutionary adaptations of certain viruses continue to pose a challenge to their long-term effectiveness.
The propensity of some viruses to develop resistance to antiviral drugs can be attributed to a combination of factors, including their inherent genetic makeup, replication strategies, and the dynamic interplay with the host's immune response.
One of the primary reasons why some viruses are more prone to developing resistance is their exceptionally high mutation rates. Viruses, unlike their more complex cellular counterparts, often lack the sophisticated proofreading mechanisms that ensure the fidelity of their genetic material during replication. This leads to the rapid accumulation of genetic variations, including those that may confer resistance to specific antiviral medications.
The human immunodeficiency virus (HIV), for instance, is renowned for its alarmingly high mutation rate, which enables it to rapidly adapt and evade the effects of antiretroviral therapies. As the virus replicates, it generates a diverse pool of genetic variants, some of which may possess mutations that render them less susceptible to the targeted antiviral drugs.
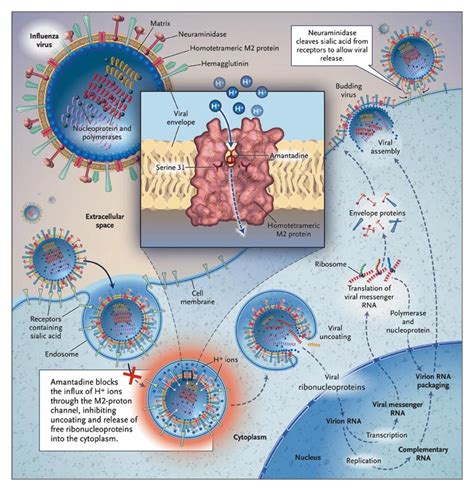
Another factor that contributes to the development of antiviral resistance is the replication strategy employed by certain viruses. Some viruses, such as influenza and hepatitis C, exhibit a rapid replication cycle and high viral loads, which increases the likelihood of random mutations occurring and the subsequent selection of resistant strains.
Furthermore, the ability of some viruses to establish persistent or latent infections within the host's cells can also complicate the effectiveness of antiviral treatments. These viruses can remain dormant for extended periods, evading the immune system and drug therapies, only to reactivate and proliferate when the conditions are favorable.
The host's immune response plays a crucial role in shaping the evolution of viral resistance as well. Certain viral infections may trigger an overzealous or dysregulated immune response, which can inadvertently create a selective pressure that favors the emergence of resistant viral variants. Conversely, a compromised or impaired immune system, as seen in immunocompromised individuals, can also contribute to the development of antiviral resistance.
Understanding the complex interplay between viruses, antiviral medications, and the host's immune system is essential for developing effective strategies to combat the growing threat of antiviral resistance. Ongoing research in areas such as viral genomics, immunology, and drug design aims to unravel the intricacies of this phenomenon, paving the way for more targeted and sustainable approaches to viral disease management.
As the battle against viral infections continues, the scientific community remains vigilant, constantly exploring new avenues to stay ahead of the ever-evolving viral foes. By understanding the factors that contribute to the development of antiviral resistance, we can work towards developing more robust and resilient therapeutic options, ultimately safeguarding the public's health and well-being.
What are your thoughts on the factors that drive the emergence of antiviral resistance? Share your insights and experiences in the comments below.