The Delicate Dance: Navigating Antiviral Drug Interactions
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-30
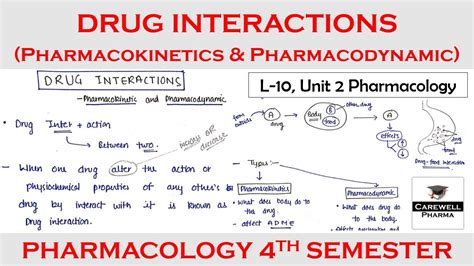
As the world continues to grapple with the impact of infectious diseases, the role of antiviral medications in managing these conditions has become increasingly crucial. However, these powerful drugs do not exist in a vacuum; their pharmacokinetic properties can be significantly influenced by the presence of other medications, leading to complex and potentially dangerous interactions.
Antivirals, a class of drugs designed to target and inhibit the replication of viruses, are often prescribed to treat a wide range of viral infections, from the common cold to life-threatening conditions like HIV and hepatitis C. These medications work by disrupting the viral life cycle, preventing the virus from effectively infecting and replicating within the host's cells. But their efficacy can be greatly impacted by the presence of other drugs, which can alter the pharmacokinetics – the absorption, distribution, metabolism, and elimination – of the antiviral agents.
One notable example is the potential interaction between antiretroviral medications used to treat HIV and certain commonly prescribed drugs, such as antibiotics, antifungals, and even some over-the-counter medications. These interactions can lead to either increased or decreased concentrations of the antiviral drug in the body, potentially resulting in reduced efficacy or an increased risk of adverse effects.
For instance, the antifungal medication ketoconazole has been shown to inhibit the metabolism of certain HIV antivirals, leading to higher drug levels and an increased risk of side effects. Conversely, the antibiotic rifampicin can enhance the metabolism of some antivirals, resulting in lower drug concentrations and potentially compromising their therapeutic effectiveness.
Similarly, the pharmacokinetics of direct-acting antiviral agents (DAAs) used to treat hepatitis C can be altered by the presence of other medications. Certain antidepressants, antiseizure drugs, and even some herbal supplements have been found to interact with DAAs, either increasing or decreasing their concentration in the body.
These complex interactions underscore the importance of careful medication management and close monitoring when prescribing antivirals. Healthcare professionals must be vigilant in identifying potential drug interactions and taking appropriate steps to mitigate the risks, such as adjusting dosages, selecting alternative medications, or closely monitoring patients for any adverse effects.
In addition to these well-documented interactions, emerging research suggests that the gut microbiome may also play a role in influencing the pharmacokinetics of antiviral medications. The diverse community of microorganisms that reside in the human gut can metabolize and transform various drugs, potentially impacting their absorption, distribution, and elimination.
As our understanding of the gut-drug axis continues to evolve, healthcare providers may need to consider the potential influence of the microbiome when managing antiviral therapy, particularly in patients with underlying gastrointestinal conditions or those who have undergone significant changes to their gut flora, such as through the use of antibiotics.
In conclusion, the intricate web of drug interactions that can affect the pharmacokinetics of antivirals highlights the importance of a comprehensive and multifaceted approach to patient care. By staying abreast of the latest research, closely monitoring patients, and collaborating with other healthcare providers, clinicians can help ensure the safe and effective use of these vital medications, ultimately improving patient outcomes and minimizing the risks associated with viral infections.
What other factors do you believe healthcare providers should consider when managing antiviral therapy and minimizing the risks of drug interactions? Share your insights and experiences in the comments below.