Unlocking the Mysteries of Antiviral Pharmacokinetics
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-18
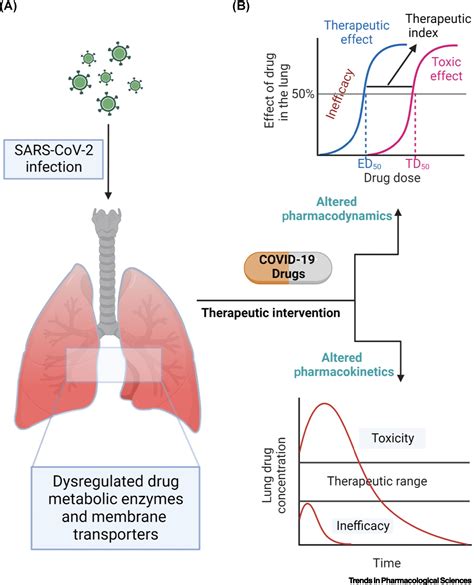
When it comes to the treatment of viral infections, antiviral drugs play a crucial role in managing the course of the disease and preventing complications. However, the effectiveness of these medications can be influenced by a complex array of factors that govern their pharmacokinetics – the way they are absorbed, distributed, metabolized, and eliminated within the human body. Understanding these factors is essential for healthcare professionals to optimize antiviral therapy and ensure the best possible outcomes for their patients.
One of the primary determinants of antiviral pharmacokinetics is the route of administration. Oral formulations, for instance, must first be absorbed through the gastrointestinal tract before reaching the systemic circulation, whereas intravenous administration allows the drug to bypass this step and enter the bloodstream directly. The rate and extent of absorption can be influenced by factors such as stomach pH, intestinal transit time, and the presence of food in the digestive system.
Another crucial factor is drug distribution, which refers to the movement of the medication throughout the body and its ability to reach the target sites of infection. The degree of protein binding, the ability of the drug to cross physiological barriers (such as the blood-brain barrier), and the presence of active transport mechanisms can all impact the distribution and subsequent concentration of the antiviral agent at the site of action.
Metabolism and elimination also play a significant role in antiviral pharmacokinetics. Hepatic metabolism, mediated by enzymes in the liver, can alter the structure and activity of the drug, potentially leading to the formation of active or inactive metabolites. The rate of renal clearance, the process by which the kidneys filter and excrete the drug or its metabolites, can also influence the overall exposure and duration of the antiviral effect.
Furthermore, patient-specific characteristics, such as age, gender, body weight, and genetic factors, can also impact antiviral pharmacokinetics. For instance, older patients may experience altered drug absorption or decreased renal function, while genetic variations in drug-metabolizing enzymes can lead to differences in the rate of drug metabolism and clearance.
Comorbidities and concomitant medications can also have a significant impact on antiviral pharmacokinetics. Underlying medical conditions, such as liver or kidney disease, can impair the body's ability to handle the drug, potentially leading to altered exposure or increased risk of adverse effects. Additionally, drug-drug interactions can occur when antiviral medications are co-administered with other therapies, potentially resulting in altered absorption, distribution, metabolism, or elimination of one or both drugs.
In conclusion, the pharmacokinetics of antiviral drugs are influenced by a complex interplay of factors, including the route of administration, drug distribution, metabolism, and elimination, as well as patient-specific characteristics and comorbidities. Understanding these factors is crucial for healthcare providers to optimize antiviral therapy, minimize the risk of adverse events, and ensure the best possible outcomes for their patients. Ongoing research and clinical studies continue to shed light on the nuances of antiviral pharmacokinetics, paving the way for more personalized and effective treatment approaches.
What other patient-specific or disease-related factors do you think might influence the pharmacokinetics of antiviral drugs?