How do Antibiotics Target Specific Bacterial Cells?
Delve into the pharmacodynamics of antibiotics and how they target specific bacterial cells. Share your knowledge on the mechanisms behind this selective action.
Antibiotics: Targeted Precision in the War Against Bacteria
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-27
The discovery of antibiotics ushered in a new era of modern medicine, revolutionizing the way we combat infectious diseases. These remarkable compounds possess the remarkable ability to selectively target and eliminate specific bacterial cells, while leaving human cells largely unharmed. But how exactly do these pharmaceutical marvels achieve this targeted precision?
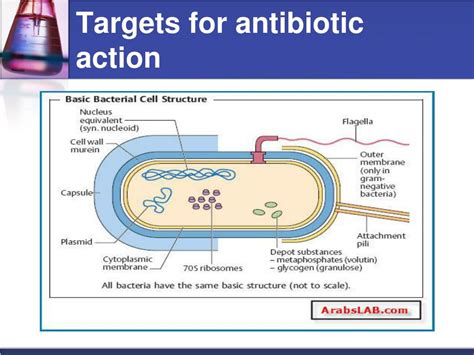
At the heart of this selective action lies the unique pharmacodynamics of antibiotics - the intricate interplay between the drug and the bacterial targets. Antibiotics have evolved to exploit the structural and functional differences between human and bacterial cells, allowing them to disrupt critical processes essential for bacterial survival and proliferation.
One of the primary mechanisms by which antibiotics target specific bacterial cells is by interfering with the synthesis of the bacterial cell wall. Many antibiotics, such as penicillins and cephalosporins, bind to and inhibit enzymes responsible for the construction and maintenance of the bacterial cell wall. This weakens the structural integrity of the cell, ultimately leading to its rupture and death.
Another common strategy employed by antibiotics is the disruption of protein synthesis within bacterial cells. Certain antibiotics, like tetracyclines and macrolides, bind to the bacterial ribosome, the cellular machinery responsible for translating genetic information into functional proteins. By impeding this process, these antibiotics effectively shut down the bacterial cell's ability to produce the essential proteins it needs to survive and thrive.
Some antibiotics, such as fluoroquinolones, target the DNA replication machinery of bacteria, interfering with the enzymes responsible for unwinding and duplicating the genetic material. This disruption in DNA replication ultimately leads to the death of the bacterial cell.
Interestingly, the selective nature of antibiotics can also be attributed to their ability to exploit unique metabolic pathways present in bacterial cells. For instance, sulfonamides and trimethoprim target the bacterial synthesis of folic acid, a critical nutrient for bacterial growth and reproduction. By selectively inhibiting this pathway, these antibiotics effectively starve the bacterial cells of a vital resource, while leaving human cells unaffected.
The remarkable selectivity of antibiotics is a testament to the evolutionary arms race between bacteria and the development of antimicrobial compounds. As bacteria continue to evolve resistance mechanisms, researchers are constantly exploring new strategies to outsmart these resilient microorganisms.
Understanding the intricate pharmacodynamics of antibiotics and their targeted mechanisms of action is crucial for the effective and responsible use of these life-saving drugs. By harnessing the power of this selective targeting, healthcare providers can tailor antibiotic treatments to specific bacterial infections, minimizing the risk of resistance and preserving the efficacy of these crucial medical tools.
As the battle against infectious diseases rages on, the continued advancement of our understanding of antibiotic pharmacodynamics will be instrumental in shaping the future of antimicrobial therapy. By unraveling the secrets of this targeted precision, we can continue to harness the power of antibiotics to protect and heal, ensuring that these remarkable compounds remain a cornerstone of modern medicine for generations to come.
User comments
More Topics to Explore
How do Antibiotics Affect Bacterial Growth Rates?
Discuss how antibiotics influence bacterial growth rates and the pharmacodynamics involved. Share your insights and knowledge on this crucial aspect of antibiotic action.
Are Antibiotics More Effective if Taken at Regular Intervals?
Delve into the importance of regular intervals in antibiotic dosing and its impact on effectiveness. Share your perspectives on the pharmacodynamics of dosing schedules.
How do Antibiotics Interact with Different Types of Bacteria?
Examine the varied interactions between antibiotics and different bacterial strains. Share examples and explanations of these pharmacodynamic interactions.
Can Antibiotics Lead to Antibiotic Resistance Through Pharmacodynamics?
Explore the fascinating connection between antibiotic use, pharmacodynamics, and the development of antibiotic resistance. Share your insights on how pharmacodynamics play a role in resistance development.
Are Peak and Trough Levels Important in Antibiotic Therapy?
Discuss the significance of peak and trough levels in antibiotic therapy and their impact on pharmacodynamics. Share your insights on monitoring these levels for optimal treatment outcomes.
Does the Route of Administration Affect Antibiotic Pharmacodynamics?
Examine how different routes of antibiotic administration can influence pharmacodynamics. Discuss the implications of administration methods on antibiotic efficacy and absorption rates.
How do Antibiotics Maintain Therapeutic Concentrations in the Body?
Dive into the mechanisms by which antibiotics sustain therapeutic concentrations in the body and their implications on pharmacodynamics. Share your understanding of how doses are optimized for efficacy.
Can Combination Antibiotic Therapy Enhance Pharmacodynamic Effects?
Explore the potential benefits of combining antibiotics to enhance pharmacodynamic effects. Share examples of synergistic interactions and the rationale behind combining different antibiotics.
Is Antibiotic Efficacy Affected by Patient Factors in Pharmacodynamics?
Discuss how patient-specific factors can influence antibiotic efficacy through pharmacodynamics. Share your insights on variables such as age, weight, and health conditions in determining treatment outcomes.