Antiviral Resistance vs. Antibiotic Resistance: A Comparative Analysis
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-25
As the world grapples with the persistent challenges of influenza and bacterial infections, the issues of antiviral resistance and antibiotic resistance have become increasingly pressing concerns for the medical community. While these two types of resistance may seem similar on the surface, a deeper examination reveals distinct mechanisms, consequences, and approaches to mitigation.
At the heart of antiviral resistance lies the ability of influenza viruses to evolve and adapt, rendering certain antiviral drugs less effective. This occurs through genetic mutations that alter the viral proteins targeted by these medications, effectively allowing the virus to evade the drug's inhibitory effects. Consequently, patients infected with resistant strains may experience reduced treatment efficacy, prolonged illness, and increased risk of complications.
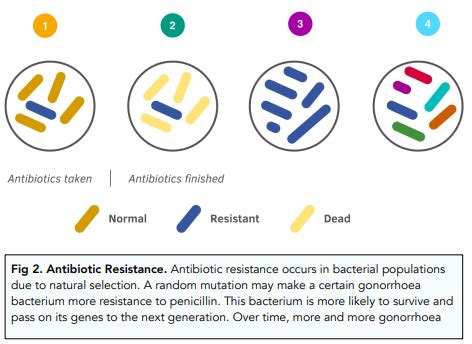
In contrast, antibiotic resistance in bacterial infections arises from the bacteria's inherent ability to adapt and develop defense mechanisms against the antibacterial compounds used to treat them. This can happen through a variety of mechanisms, such as the production of enzymes that inactivate the antibiotics, modifications of the drug's target site, or the acquisition of resistance genes from other bacteria. The consequences of antibiotic resistance are equally concerning, as it can lead to the failure of standard treatment regimens, increased hospitalizations, and the potential spread of untreatable infections.
One notable similarity between antiviral and antibiotic resistance is the role of selective pressure in their development. Both influenza viruses and bacteria can rapidly replicate and evolve, with each new generation presenting an opportunity for advantageous mutations to arise and proliferate. The widespread and sometimes indiscriminate use of antiviral drugs and antibiotics has contributed to this selective pressure, favoring the survival and propagation of resistant strains.
However, a key difference lies in the nature of the pathogens themselves. Viruses, such as influenza, are obligate intracellular parasites, meaning they rely on the host's cellular machinery to replicate and spread. This dependency on the host's resources can limit the options for antiviral drug development, as targeting the virus without harming the host cells can be a delicate balance. In contrast, bacteria are independent, free-living organisms, which provides more opportunities for the development of targeted antibacterial therapies.
To combat the rising tide of antiviral and antibiotic resistance, a multifaceted and interdisciplinary approach is required. Continued research into the mechanisms of resistance, the development of novel antiviral and antibiotic compounds, and the optimization of existing treatments are all crucial components of this effort. Additionally, improved infection prevention and control measures, antimicrobial stewardship programs, and public education initiatives can help mitigate the spread of resistant pathogens and preserve the efficacy of our current therapeutic arsenal.
As we navigate the complexities of antiviral and antibiotic resistance, it is clear that collaborative efforts between medical professionals, researchers, and policymakers will be essential in safeguarding the health and well-being of individuals and communities worldwide. By embracing a comprehensive understanding of these challenges, we can work towards a future where the battle against infectious diseases is fought with greater effectiveness and resilience.