Antiviral Resistance Patterns in Influenza: What Can We Learn?
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-22
As the world grapples with the ever-evolving threat of influenza, a growing concern has emerged around the patterns of antiviral resistance among circulating strains. This complex issue holds significant implications for public health strategies, treatment protocols, and the development of new antiviral agents.
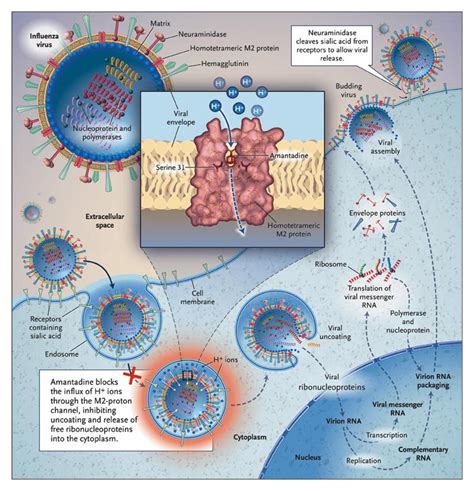
Influenza, a highly contagious respiratory illness, is caused by viruses that can mutate rapidly, often rendering existing treatments less effective. The two main classes of antiviral drugs used to manage influenza are the neuraminidase inhibitors (e.g., oseltamivir, zanamivir) and the adamantanes (e.g., amantadine, rimantadine). While these medications have proven effective in the past, the emergence of resistant strains has posed a significant challenge to healthcare professionals.
Global surveillance data has revealed a complex and ever-changing landscape of antiviral resistance patterns. In recent years, certain H1N1 and H3N2 influenza strains have exhibited increased resistance to neuraminidase inhibitors, rendering these once-reliable treatments less effective. Additionally, the adamantanes have faced widespread resistance, with the majority of circulating strains demonstrating resistance to these drugs.
These patterns of resistance have profound implications for public health. Clinicians must carefully consider the local and regional resistance patterns when prescribing antiviral medications, as the efficacy of these drugs can vary significantly based on the predominant strains in a given area. This, in turn, affects the development of treatment protocols and public health strategies, as healthcare systems must adapt to the evolving landscape of antiviral resistance.
Furthermore, the emergence of resistant strains has highlighted the pressing need for the development of new antiviral agents. Researchers and pharmaceutical companies are actively exploring innovative approaches to combat the threat of influenza, including the development of novel drug targets, combination therapies, and the exploration of alternative mechanisms of action.
One promising avenue of research is the investigation of polymerase inhibitors, which target the viral enzymes responsible for genome replication and transcription. These drugs hold the potential to be less vulnerable to the rapid mutations that often confer resistance to neuraminidase and adamantane inhibitors.
Another area of focus is the development of monoclonal antibodies, which can recognize and neutralize specific influenza strains. These targeted therapies could potentially overcome the challenge of antiviral resistance by targeting conserved regions of the virus that are less prone to mutation.
As the global community continues to grapple with the ever-evolving threat of influenza, the study of antiviral resistance patterns holds the key to informed decision-making and the development of more effective treatment and prevention strategies. By understanding the complex dynamics of resistance, healthcare professionals and researchers can work to stay one step ahead of the virus, ultimately safeguarding public health and enhancing our preparedness for future influenza outbreaks.
What insights can we gain from the current patterns of antiviral resistance, and how might these findings shape the future of influenza management?