How can individuals help combat community-acquired antibiotic resistance?
Discuss ways in which individuals can actively contribute to reducing antibiotic resistance in community settings and promoting responsible antibiotic use.
Community-Acquired Antibiotic Resistance: What Can Individuals Do?
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Apr-09
Antibiotic resistance is a growing public health concern, with increasing rates of community-acquired infections caused by drug-resistant pathogens. As individuals, we may feel powerless in the face of this complex issue, but in reality, our everyday choices and actions can make a meaningful difference in combating this challenge.
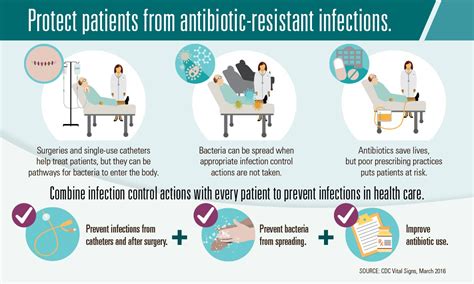
At the core of community-acquired antibiotic resistance lies the overuse and misuse of these vital medications. Antibiotics are often prescribed unnecessarily for viral infections, where they provide no benefit, or are not taken as directed. This fuels the evolution of resistant bacteria, rendering these life-saving drugs less effective when they are truly needed.
One crucial step individuals can take is to become more informed antibiotic stewards. When experiencing symptoms of an illness, resist the temptation to demand antibiotics from your healthcare provider. Instead, have an open dialogue about whether antibiotics are the appropriate course of treatment. Understand that some infections, such as the common cold or influenza, are viral in nature and do not require antibiotics. By exercising patience and allowing your body's immune system to fight off minor infections, you can help curb the spread of antibiotic resistance.
Furthermore, when antibiotics are prescribed, it is essential to adhere strictly to the dosage instructions and complete the full course of treatment. Skipping doses or stopping the medication prematurely can allow surviving bacteria to develop resistance, undermining the effectiveness of the drug.
Beyond responsible personal use, individuals can also advocate for public health policies that promote judicious antibiotic prescribing. Support legislation and regulations that restrict the use of antibiotics in agriculture, where they are often used indiscriminately to promote growth in livestock. Urge your healthcare providers and local government officials to implement stewardship programs that educate both medical professionals and the general public on the importance of appropriate antibiotic use.
In the community setting, individuals can also play a role in preventing the spread of resistant infections. Proper hand hygiene, through frequent and thorough handwashing with soap and water or the use of alcohol-based hand sanitizers, can limit the transmission of harmful bacteria. Additionally, staying up-to-date with recommended vaccinations can help protect yourself and your loved ones from infections that might otherwise require antibiotic treatment.
Community engagement and education are also vital in the fight against antibiotic resistance. Reach out to local schools, community centers, or healthcare facilities and volunteer to participate in educational initiatives that raise awareness about this issue. By sharing accurate information and dispelling misconceptions, you can empower your fellow community members to make informed decisions about antibiotic use.
In the face of this growing public health challenge, individual actions may seem small, but they can have a profound impact when multiplied across communities. By embracing our roles as responsible antibiotic stewards, we can collectively work to preserve the effectiveness of these crucial medications and safeguard the health of our communities for generations to come. What steps will you take to combat community-acquired antibiotic resistance?
User comments
More Topics to Explore
How can we prevent community-acquired antibiotic resistance?
Discuss strategies for preventing antibiotic resistance in community settings and share effective prevention methods.
Are there specific antibiotics more prone to community-acquired resistance?
Explore the antibiotics that are more susceptible to resistance in community settings and discuss reasons behind this trend.
What role do healthcare professionals play in combatting community-acquired antibiotic resistance?
Analyze the impact and responsibilities of healthcare providers in fighting antibiotic resistance in community-acquired infections.
How does poor sanitation contribute to community-acquired antibiotic resistance?
Examine the relationship between inadequate sanitation practices and the development of antibiotic resistance in community settings.
What are the consequences of untreated community-acquired antibiotic-resistant infections?
Delve into the potential outcomes and risks associated with untreated antibiotic-resistant infections in the community.
Can education and awareness campaigns help reduce community-acquired antibiotic resistance?
Debate the effectiveness of educational initiatives and awareness campaigns in lowering antibiotic resistance rates in community-acquired infections.
Is livestock farming a contributing factor to community-acquired antibiotic resistance?
Investigate the potential influence of livestock farming practices on the development of antibiotic resistance in the community.
What are the challenges in diagnosing community-acquired antibiotic-resistant infections?
Highlight the difficulties and obstacles healthcare professionals face when diagnosing antibiotic-resistant infections in the community.
What are the current trends in community-acquired antibiotic resistance?
Explore the latest patterns and developments in antibiotic resistance within community settings and discuss emerging trends.