Is livestock farming a contributing factor to community-acquired antibiotic resistance?
Investigate the potential influence of livestock farming practices on the development of antibiotic resistance in the community.
The Troubling Link Between Livestock Farming and Antibiotic Resistance
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Apr-02
As our reliance on antibiotics has grown, so too has the concerning rise of antibiotic resistance within our communities. While many factors likely contribute to this alarming trend, a growing body of evidence suggests that the practices of livestock farming may be playing a significant role.
The use of antibiotics in animal agriculture is widespread, with estimates indicating that up to 80% of antibiotics sold in the United States are used for livestock. These drugs are often administered not only to treat sick animals, but also preemptively to promote growth and prevent disease in healthy herds. This prophylactic use, however, creates the perfect conditions for resistant bacteria to emerge and proliferate.
When antibiotics are overused, whether in humans or animals, the natural selection process favors bacteria that have developed mechanisms to survive the drugs' effects. Over time, these resilient microbes can spread beyond the farm, hitchhiking on animals, farm equipment, runoff water, or workers. Studies have found antibiotic-resistant bacteria isolated from livestock operations in the surrounding environment, contaminating the soil, air, and water sources that local communities rely on.
Moreover, the sheer scale of industrial animal agriculture amplifies the problem. Intensive, crowded living conditions on many modern farms allow resistant pathogens to rapidly transmit between animals, creating a veritable breeding ground for new resistant strains. As these bacteria spread, they can then be passed on to humans through direct contact, the food supply, or other environmental exposure.
The public health implications are significant. Antibiotic-resistant infections are notoriously difficult to treat, leading to prolonged illnesses, increased hospitalization rates, and higher mortality. Researchers have found direct links between the use of certain antibiotics in livestock and the emergence of resistant variants in human populations living near these farms. This underscores the complex, bidirectional relationship between agricultural and clinical antibiotic use.
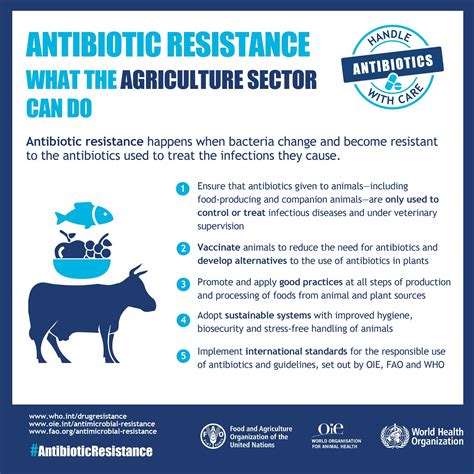
Addressing this challenge will require a multifaceted approach. Improved biosecurity measures, restricted antibiotic use, and a shift towards more sustainable farming practices that prioritize animal welfare could all help mitigate the spread of resistant bacteria. Increased monitoring and data-sharing between the agricultural and medical communities will also be crucial for identifying emerging threats and implementing targeted interventions.
As we continue to grapple with the growing crisis of antibiotic resistance, it is clear that the practices of livestock farming can no longer be considered in isolation. Understanding and addressing this sector's contribution to the problem will be key to safeguarding public health for generations to come. What other steps do you believe could help break the cycle of resistance stemming from animal agriculture?
User comments
More Topics to Explore
How can we prevent community-acquired antibiotic resistance?
Discuss strategies for preventing antibiotic resistance in community settings and share effective prevention methods.
Are there specific antibiotics more prone to community-acquired resistance?
Explore the antibiotics that are more susceptible to resistance in community settings and discuss reasons behind this trend.
What role do healthcare professionals play in combatting community-acquired antibiotic resistance?
Analyze the impact and responsibilities of healthcare providers in fighting antibiotic resistance in community-acquired infections.
How does poor sanitation contribute to community-acquired antibiotic resistance?
Examine the relationship between inadequate sanitation practices and the development of antibiotic resistance in community settings.
What are the consequences of untreated community-acquired antibiotic-resistant infections?
Delve into the potential outcomes and risks associated with untreated antibiotic-resistant infections in the community.
Can education and awareness campaigns help reduce community-acquired antibiotic resistance?
Debate the effectiveness of educational initiatives and awareness campaigns in lowering antibiotic resistance rates in community-acquired infections.
What are the challenges in diagnosing community-acquired antibiotic-resistant infections?
Highlight the difficulties and obstacles healthcare professionals face when diagnosing antibiotic-resistant infections in the community.
How can individuals help combat community-acquired antibiotic resistance?
Discuss ways in which individuals can actively contribute to reducing antibiotic resistance in community settings and promoting responsible antibiotic use.
What are the current trends in community-acquired antibiotic resistance?
Explore the latest patterns and developments in antibiotic resistance within community settings and discuss emerging trends.