How can we prevent community-acquired antibiotic resistance?
Discuss strategies for preventing antibiotic resistance in community settings and share effective prevention methods.
The Growing Threat of Antibiotic Resistance in Our Communities
Posted by Rick Ashworth, reviewed by Dr. Miguel Sanchez | 2024-Mar-15
The overuse and misuse of antibiotics has become a critical public health issue, leading to the alarming rise of antibiotic-resistant bacteria in community settings. As these superbugs become more prevalent, it is imperative that we take proactive steps to prevent the further spread of community-acquired antibiotic resistance.
One of the primary drivers of this problem is the casual attitude many people have towards taking antibiotics. Far too often, individuals demand antibiotics from their doctors for viral infections that do not respond to these medications. This fuels the evolution of resistant strains, as the antibiotics kill off susceptible bacteria while allowing hardier variants to thrive and proliferate. Educating the public on the proper use of antibiotics, and the dangers of overuse, will be crucial in curbing this dangerous trend.
Healthcare professionals also have an important role to play. Doctors must be more judicious in prescribing antibiotics, reserving them only for bacterial infections where they are truly warranted. This requires a commitment to evidence-based practices and a willingness to have frank conversations with patients about when antibiotics are - and are not - an appropriate treatment. Pharmacists, too, can help by ensuring patients understand dosage instructions and the importance of completing the full course of medication.
Beyond improving antibiotic stewardship, enhanced infection prevention and control measures in the community are vital. Thorough and frequent handwashing, especially before preparing food or caring for the sick, can dramatically reduce the transmission of harmful bacteria. Vaccination programs that protect against common infections can also diminish the need for antibiotics. And proper cleaning and disinfection of shared public spaces, from schools to grocery stores, makes it harder for resistant microbes to spread.
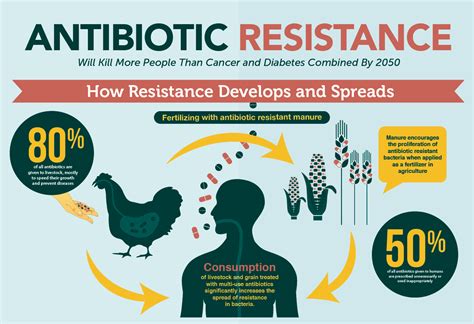
The agricultural sector bears responsibility as well. The routine use of antibiotics in livestock farming has been linked to the emergence of resistant bacteria that can then infect humans. Transitioning to more sustainable, antibiotic-free farming practices is crucial to address this problem at the source.
Ultimately, combating community-acquired antibiotic resistance will require a multipronged, collaborative approach involving patients, healthcare providers, policymakers, and industry. It will take time and concerted effort, but the stakes are too high to ignore this growing threat.
What other strategies do you think could be effective in preventing the spread of resistant bacteria in our communities? Share your thoughts and insights below.
User comments
More Topics to Explore
Are there specific antibiotics more prone to community-acquired resistance?
Explore the antibiotics that are more susceptible to resistance in community settings and discuss reasons behind this trend.
What role do healthcare professionals play in combatting community-acquired antibiotic resistance?
Analyze the impact and responsibilities of healthcare providers in fighting antibiotic resistance in community-acquired infections.
How does poor sanitation contribute to community-acquired antibiotic resistance?
Examine the relationship between inadequate sanitation practices and the development of antibiotic resistance in community settings.
What are the consequences of untreated community-acquired antibiotic-resistant infections?
Delve into the potential outcomes and risks associated with untreated antibiotic-resistant infections in the community.
Can education and awareness campaigns help reduce community-acquired antibiotic resistance?
Debate the effectiveness of educational initiatives and awareness campaigns in lowering antibiotic resistance rates in community-acquired infections.
Is livestock farming a contributing factor to community-acquired antibiotic resistance?
Investigate the potential influence of livestock farming practices on the development of antibiotic resistance in the community.
What are the challenges in diagnosing community-acquired antibiotic-resistant infections?
Highlight the difficulties and obstacles healthcare professionals face when diagnosing antibiotic-resistant infections in the community.
How can individuals help combat community-acquired antibiotic resistance?
Discuss ways in which individuals can actively contribute to reducing antibiotic resistance in community settings and promoting responsible antibiotic use.
What are the current trends in community-acquired antibiotic resistance?
Explore the latest patterns and developments in antibiotic resistance within community settings and discuss emerging trends.